Search
- Page Path
- HOME > Search
- Thyroid
Big Data Articles (National Health Insurance Service Database) - Prevalence, Treatment Status, and Comorbidities of Hyperthyroidism in Korea from 2003 to 2018: A Nationwide Population Study
- Hwa Young Ahn, Sun Wook Cho, Mi Young Lee, Young Joo Park, Bon Seok Koo, Hang-Seok Chang, Ka Hee Yi
- Endocrinol Metab. 2023;38(4):436-444. Published online July 12, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1684
- 1,808 View
- 127 Download
- 1 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
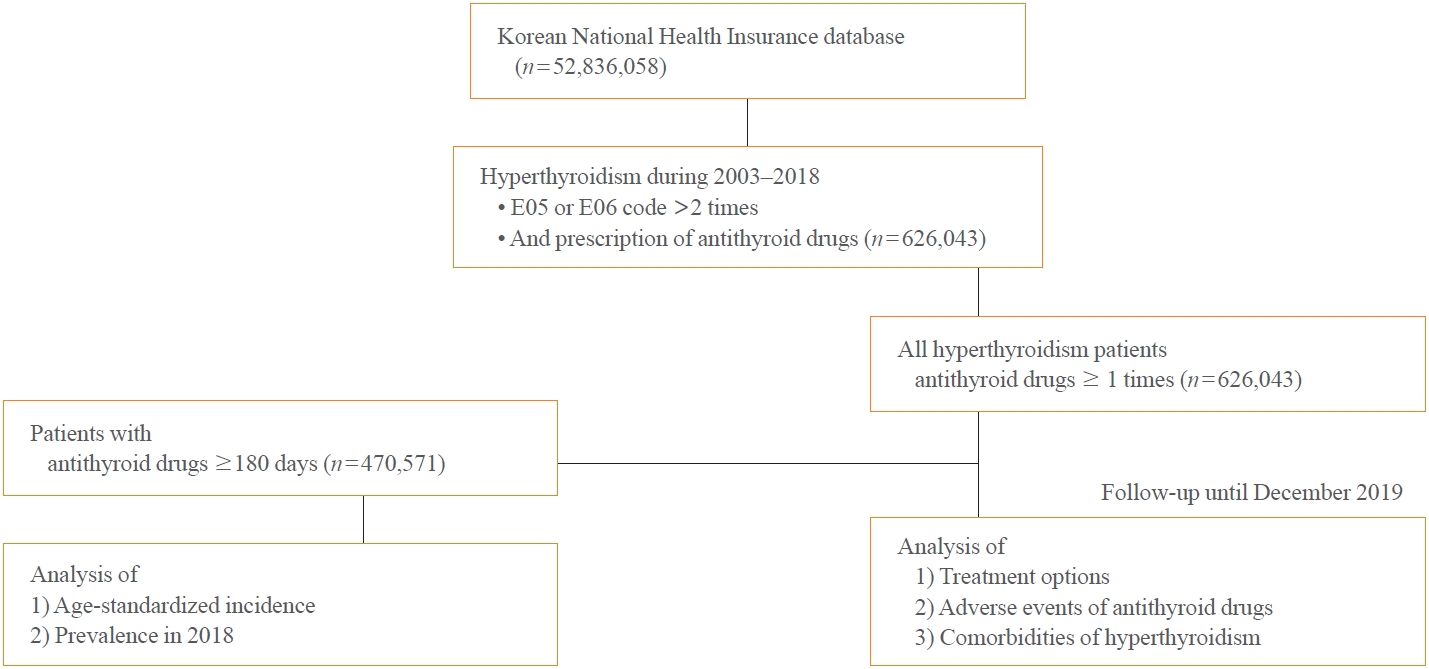
This study aimed to investigate the changes of incidence and treatment of choice for hyperthyroidism from 2003 to 2018 and explore the treatment-related complications and concomitant comorbidities in South Korea using data from the National Health Insurance Service.
Methods
This is a retrospective observational study. Hyperthyroidism was defined as a case having two or more diagnostic codes of thyrotoxicosis, with antithyroid drug intake for more than 6 months.
Results
The average age-standardized incidence of hyperthyroidism from 2003 to 2018 was 42.23 and 105.13 per 100,000 men and women, respectively. In 2003 to 2004, hyperthyroidism was most often diagnosed in patients in their 50s, but in 2017 to 2018, people were most often diagnosed in their 60s. During the entire period, about 93.7% of hyperthyroidism patients were prescribed with antithyroid drugs, and meanwhile, the annual rates of ablation therapy decrease from 7.68% in 2008 to 4.56% in 2018. Antithyroid drug-related adverse events, mainly agranulocytosis and acute hepatitis, as well as complications of hyperthyroidism such as atrial fibrillation or flutter, osteoporosis, and fractures, occurred more often in younger patients.
Conclusion
In Korea, hyperthyroidism occurred about 2.5 times more in women than in men, and antithyroid drugs were most preferred as the first-line treatment. Compared to the general population, hyperthyroid patients may have a higher risk of atrial fibrillation or flutter, osteoporosis, and fractures at a younger age. -
Citations
Citations to this article as recorded by- Long-term effect of thyrotropin-binding inhibitor immunoglobulin on atrial fibrillation in euthyroid patients
Jung-Chi Hsu, Kang-Chih Fan, Ting-Chuan Wang, Shu-Lin Chuang, Ying-Ting Chao, Ting-Tse Lin, Kuan-Chih Huang, Lian-Yu Lin, Lung-Chun Lin
Endocrine Practice.2024;[Epub] CrossRef - The Current Status of Hyperthyroidism in Korea
Hyemi Kwon
Endocrinology and Metabolism.2023; 38(4): 392. CrossRef - Is Thyroid Dysfunction Associated with Unruptured Intracranial Aneurysms? A Population-Based, Nested Case–Control Study from Korea
Hyeree Park, Sun Wook Cho, Sung Ho Lee, Kangmin Kim, Hyun-Seung Kang, Jeong Eun Kim, Aesun Shin, Won-Sang Cho
Thyroid®.2023; 33(12): 1483. CrossRef
- Long-term effect of thyrotropin-binding inhibitor immunoglobulin on atrial fibrillation in euthyroid patients

- Thyroid
- Diagnosis and Management of Thyroid Disease during Pregnancy and Postpartum: 2023 Revised Korean Thyroid Association Guidelines
- Hwa Young Ahn, Ka Hee Yi
- Endocrinol Metab. 2023;38(3):289-294. Published online June 9, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1696
- 6,500 View
- 706 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
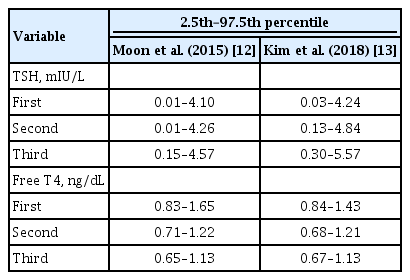
ePub - Thyroid hormone plays a critical role in fetal growth and development, and thyroid dysfunction during pregnancy is associated with several adverse outcomes, such as miscarriage and preterm birth. In this review, we introduce and explain three major changes in the revised Korean Thyroid Association (KTA) guidelines for the diagnosis and management of thyroid disease during pregnancy: first, the normal range of thyroid-stimulating hormone (TSH) during pregnancy; second, the treatment of subclinical hypothyroidism; and third, the management of euthyroid pregnant women with positive thyroid autoantibodies. The revised KTA guidelines adopt 4.0 mIU/L as the upper limit of TSH in the first trimester. A TSH level between 4.0 and 10.0 mIU/L, combined with free thyroxine (T4) within the normal range, is defined as subclinical hypothyroidism, and a TSH level over 10 mIU/L is defined as overt hypothyroidism regardless of the free T4 level. Levothyroxine treatment is recommended when the TSH level is higher than 4 mIU/L in subclinical hypothyroidism, regardless of thyroid peroxidase antibody positivity. However, thyroid hormone therapy to prevent miscarriage is not recommended in thyroid autoantibody-positive women with normal thyroid function.
-
Citations
Citations to this article as recorded by- Use of thyroid hormones in hypothyroid and euthyroid patients: A survey of members of the Endocrine Society of Australia
Nicole Lafontaine, Suzanne J. Brown, Petros Perros, Enrico Papini, Endre V. Nagy, Roberto Attanasio, Laszlo Hegedüs, John P. Walsh
Clinical Endocrinology.2024; 100(5): 477. CrossRef - Management of Subclinical Hypothyroidism: A Focus on Proven Health Effects in the 2023 Korean Thyroid Association Guidelines
Eu Jeong Ku, Won Sang Yoo, Hyun Kyung Chung
Endocrinology and Metabolism.2023; 38(4): 381. CrossRef - Maternal isolated hypothyroxinemia in the first trimester is not associated with adverse pregnancy outcomes, except for macrosomia: a prospective cohort study in China
Jing Du, Linong Ji, Xiaomei Zhang, Ning Yuan, Jianbin Sun, Dan Zhao
Frontiers in Endocrinology.2023;[Epub] CrossRef
- Use of thyroid hormones in hypothyroid and euthyroid patients: A survey of members of the Endocrine Society of Australia

- Thyroid
Thyroid Cancer Screening - The 2017 United States Preventive Services Task Force Recommendation for Thyroid Cancer Screening Is No Longer the Gold Standard
- Ka Hee Yi
- Endocrinol Metab. 2023;38(1):72-74. Published online February 27, 2023
- DOI: https://doi.org/10.3803/EnM.2023.106
- 1,026 View
- 82 Download

- Thyroid
- Clinicopathological Characteristics and Recurrence-Free Survival of Rare Variants of Papillary Thyroid Carcinomas in Korea: A Retrospective Study
- Mijin Kim, Sun Wook Cho, Young Joo Park, Hwa Young Ahn, Hee Sung Kim, Yong Joon Suh, Dughyun Choi, Bu Kyung Kim, Go Eun Yang, Il-Seok Park, Ka Hee Yi, Chan Kwon Jung, Bo Hyun Kim
- Endocrinol Metab. 2021;36(3):619-627. Published online June 10, 2021
- DOI: https://doi.org/10.3803/EnM.2021.974

- 4,698 View
- 180 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
We aimed to evaluate the clinicopathological features and biological behaviors of Korean thyroid cancer patients with rare variants of papillary thyroid carcinoma (PTC) to address the ambiguity regarding the prognostic consequences of these variants.
Methods
We retrospectively reviewed the medical records of 5,496 patients who underwent thyroid surgery for PTC, between January and December 2012, in nine tertiary hospitals. Rare PTC variants included tall cell (TCV), columnar cell (CCV), diffuse sclerosing (DSV), cribriform-morular (CMV), solid (SV), hobnail, and Warthin-like variants. Recurrence-free survival (RFS) was defined as the time from the date of thyroidectomy until recurrence.
Results
Rare variants accounted for 1.1% (n=63) of the PTC patients; with 0.9% TCV, 0.02% CCV, 0.1% DSV, 0.1% CMV, and 0.1% SV. The mean age of patients and primary tumor size were 42.1±13.1 years and 1.3±0.9 cm, respectively. Extrathyroidal extension and cervical lymph node metastasis were observed in 38 (60.3%) and 37 (58.7%) patients, respectively. Ultrasonographic findings revealed typical malignant features in most cases. During a median follow-up of 7 years, 6.3% of patients experienced a locoregional recurrence. The 5-year RFS rates were 71.4% in patients with DSV or SV, 95.9% for TCV, or CCV, and 100% for other variants. DSV emerged an independent risk factor associated with shorter RFS.
Conclusion
In this multicenter Korean cohort, rare variants accounted for 1.1% of all PTC cases, with TCV being the most frequent subtype. DSV emerged as a significant prognostic factor for RFS. -
Citations
Citations to this article as recorded by- Serum thyroglobulin testing after thyroid lobectomy in patients with 1–4 cm papillary thyroid carcinoma
Ahreum Jang, Meihua Jin, Chae A Kim, Min Ji Jeon, Yu-Mi Lee, Tae-Yon Sung, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Won Gu Kim
Endocrine.2023; 81(2): 290. CrossRef - Do Histologically Aggressive Subtypes of Papillary Thyroid
Microcarcinoma have Worse Clinical Outcome than Non-Aggressive Papillary Thyroid
Microcarcinoma Subtypes? A Multicenter Cohort Study
Sayid Shafi Zuhur, Hunkar Aggul, Ugur Avci, Selvinaz Erol, Mazhar Müslüm Tuna, Serhat Uysal, Gulhan Akbaba, Faruk Kilinç, Merve Catak, Sakin Tekin, Ogun Irem Bilen, Beyza Olcay Öztürk, Ecem Bilgehan Erden, Gulsah Elbuken, Halise Cinar Yavuz, Pinar Kadiogl
Hormone and Metabolic Research.2023; 55(05): 323. CrossRef - The Warthin-like variant of papillary thyroid carcinomas: a clinicopathologic analysis report of two cases
Xing Zhao, Yijia Zhang, Pengyu Hao, Mingzhen Zhao, Xingbin Shen
Oncologie.2023; 25(5): 581. CrossRef - A Retrospective Cohort Study with Validation of Predictors of Differentiated Thyroid Cancer Outcomes
Ayanthi Wijewardene, Anthony J. Gill, Matti Gild, Diana L. Learoyd, Anthony Robert Glover, Mark Sywak, Stan Sidhu, Paul Roach, Geoffrey Schembri, Jeremy Hoang, Bruce Robinson, Lyndal Tacon, Roderick Clifton-Bligh
Thyroid.2022;[Epub] CrossRef - Clinicopathological Implications of the BRAFV600E Mutation in Papillary Thyroid Carcinoma of Ukrainian Patients Exposed to the Chernobyl Radiation in Childhood: A Study for 30 Years After the Accident
Liudmyla Zurnadzhy, Tetiana Bogdanova, Tatiana I. Rogounovitch, Masahiro Ito, Mykola Tronko, Shunichi Yamashita, Norisato Mitsutake, Michael Bolgov, Serhii Chernyshov, Sergii Masiuk, Vladimir A. Saenko
Frontiers in Medicine.2022;[Epub] CrossRef
- Serum thyroglobulin testing after thyroid lobectomy in patients with 1–4 cm papillary thyroid carcinoma

- Thyroid
- Effect of Cigarette Smoking on Thyroid Cancer: Meta-Analysis
- Joon-Hyop Lee, Young Jun Chai, Ka Hee Yi
- Endocrinol Metab. 2021;36(3):590-598. Published online May 26, 2021
- DOI: https://doi.org/10.3803/EnM.2021.954

- 12,536 View
- 191 Download
- 8 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Although smoking is generally carcinogenic, its effect on thyroid cancers is still subject to controversy. The purpose of this study was to summarize the role of smoking in relation to thyroid cancer occurrence.
Methods
We performed a meta-analysis of 24 eligible studies: 21 case-control studies and three prospective cohort studies. The summary odds ratio (OR) and 95% confidence interval (CI) of all studies were acquired based on random effect model. Further subgroup analyses were conducted according to gender, histological type of thyroid cancer, and smoking status of patients for the case-control studies.
Results
The summary effect size indicated a negative association of smoking for thyroid cancer (OR, 0.798; 95% CI, 0.681 to 0.935). From the subgroup analyses for the case-control studies, reduced risk of thyroid cancer was observed in both men (OR, 0.734; 95% CI, 0.553 to 0.974) and women (OR, 0.792; 95% CI, 0.700 to 0.897). The protective effect of smoking was observed in studies in which thyroid cancer was limited to differentiated thyroid cancers (DTCs) (OR, 0.798; 95% CI, 0.706 to 0.902).
Conclusion
Our results suggests that smoking may have a protective effect on thyroid cancer, especially on DTCs. Further studies with larger sample sizes should be conducted in elucidating the dose and time dependent effect of smoking on thyroid cancer with specific focus on the types of thyroid cancers. -
Citations
Citations to this article as recorded by- Tobacco smoking, e-cigarette and thyroid: what are the risks of thyroid disorders
I. M. Belovalova, E. S. Shugurova, M. O. Korchagina, T. N. Borkhoeva, M. S. Sheremeta
Clinical and experimental thyroidology.2024; 19(2): 11. CrossRef - Relationship between Serum Levels of Selenium and Thyroid Cancer: A Systematic Review and Meta-Analysis
Runhua Hao, Ping Yu, Lanlan Gui, Niannian Wang, Da Pan, Shaokang Wang
Nutrition and Cancer.2023; 75(1): 14. CrossRef - Potentially inappropriate medication and frailty in older adults: A systematic review and meta-analysis
Wenlian Ma, Hongyan Wang, Zhifei Wen, Linfeng Liu, Xiangeng Zhang
Archives of Gerontology and Geriatrics.2023; 114: 105087. CrossRef - Inflammation biomarkers are associated with the incidence of cardiovascular disease: a meta-analysis
Yifei Liu, Suzhen Guan, Haiming Xu, Na Zhang, Min Huang, Zhihong Liu
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Maternal gestational weight gain and offspring’s neurodevelopmental outcomes: A systematic review and meta-analysis
Dan Wu, Yicheng Li, Lingyan Chen, Marieke Klein, Barbara Franke, Jinjin Chen, Jan Buitelaar
Neuroscience & Biobehavioral Reviews.2023; 153: 105360. CrossRef - Association of preoperative hypoprotein malnutrition with spinal postoperative complications and other conditions: A systematic review and meta-analysis
Yongrong Hu, Liping Wang, Hao Liu, Kunhai Yang, Song Wang, Xiang Zhang, Bo Qu, Hongsheng Yang
Clinical Nutrition ESPEN.2023; 57: 448. CrossRef - Metabolic syndrome and risk of ovarian cancer: a systematic review and meta-analysis
Ziyu Chen, Zesi Liu, Hongxia Yang, Chaosheng Liu, Fandou Kong
Frontiers in Endocrinology.2023;[Epub] CrossRef - Cigarette smoking and thyroid cancer risk: A Mendelian randomization study
Hongzhan Jiang, Yi Li, Jiali Shen, Huihui Lin, Siyue Fan, Rongliang Qiu, Jiaxi He, Ende Lin, Lijuan Chen
Cancer Medicine.2023; 12(19): 19866. CrossRef - Longitudinal Changes in Smoking Habits in Women and Subsequent Risk of Cancer
Thi Xuan Mai Tran, Soyeoun Kim, Huiyeon Song, Boyoung Park
American Journal of Preventive Medicine.2022; 63(6): 894. CrossRef
- Tobacco smoking, e-cigarette and thyroid: what are the risks of thyroid disorders

- Thyroid
- A Multicenter, Randomized, Controlled Trial for Assessing the Usefulness of Suppressing Thyroid Stimulating Hormone Target Levels after Thyroid Lobectomy in Low to Intermediate Risk Thyroid Cancer Patients (MASTER): A Study Protocol
- Eun Kyung Lee, Yea Eun Kang, Young Joo Park, Bon Seok Koo, Ki-Wook Chung, Eu Jeong Ku, Ho-Ryun Won, Won Sang Yoo, Eonju Jeon, Se Hyun Paek, Yong Sang Lee, Dong Mee Lim, Yong Joon Suh, Ha Kyoung Park, Hyo-Jeong Kim, Bo Hyun Kim, Mijin Kim, Sun Wook Kim, Ka Hee Yi, Sue K. Park, Eun-Jae Jung, June Young Choi, Ja Seong Bae, Joon Hwa Hong, Kee-Hyun Nam, Young Ki Lee, Hyeong Won Yu, Sujeong Go, Young Mi Kang, MASTER study group
- Endocrinol Metab. 2021;36(3):574-581. Published online May 26, 2021
- DOI: https://doi.org/10.3803/EnM.2020.943
- 6,294 View
- 268 Download
- 8 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
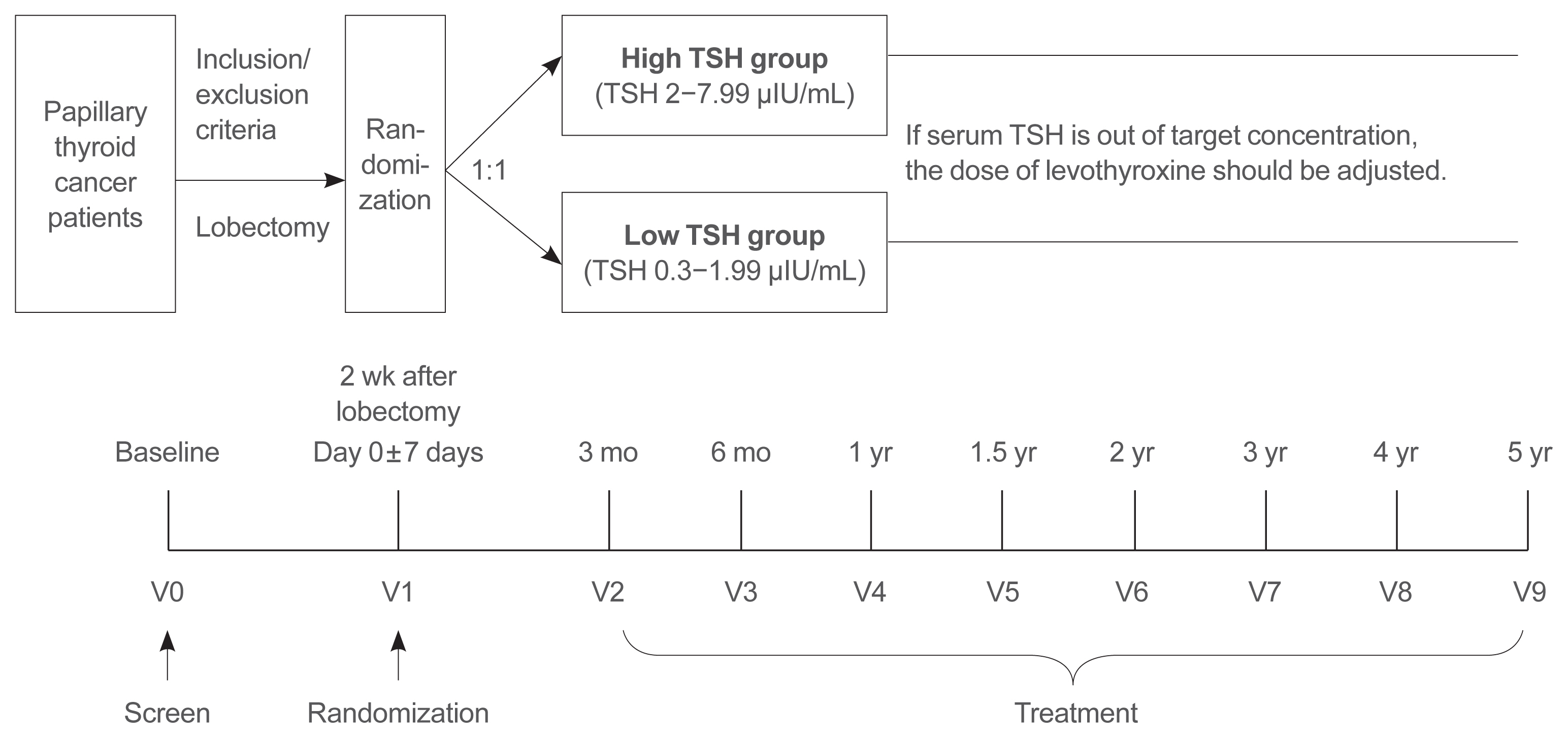
Postoperative thyroid stimulating hormone (TSH) suppression therapy is recommended for patients with intermediate- and high-risk differentiated thyroid cancer to prevent the recurrence of thyroid cancer. With the recent increase in small thyroid cancer cases, the extent of resection during surgery has generally decreased. Therefore, questions have been raised about the efficacy and long-term side effects of TSH suppression therapy in patients who have undergone a lobectomy.
Methods
This is a multicenter, prospective, randomized, controlled clinical trial in which 2,986 patients with papillary thyroid cancer are randomized into a high-TSH group (intervention) and a low-TSH group (control) after having undergone a lobectomy. The principle of treatment includes a TSH-lowering regimen aimed at TSH levels between 0.3 and 1.99 μIU/mL in the low-TSH group. The high-TSH group targets TSH levels between 2.0 and 7.99 μIU/mL. The dose of levothyroxine will be adjusted at each visit to maintain the target TSH level. The primary outcome is recurrence-free survival, as assessed by neck ultrasound every 6 to 12 months. Secondary endpoints include disease-free survival, overall survival, success rate in reaching the TSH target range, the proportion of patients with major cardiovascular diseases or bone metabolic disease, the quality of life, and medical costs. The follow-up period is 5 years.
Conclusion
The results of this trial will contribute to establishing the optimal indication for TSH suppression therapy in low-risk papillary thyroid cancer patients by evaluating the benefit and harm of lowering TSH levels in terms of recurrence, metabolic complications, costs, and quality of life. -
Citations
Citations to this article as recorded by- Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study)
Ja Kyung Lee, Eu Jeong Ku, Su-jin Kim, Woochul Kim, Jae Won Cho, Kyong Yeun Jung, Hyeong Won Yu, Yea Eun Kang, Mijin Kim, Hee Kyung Kim, Junsun Ryu, June Young Choi
Annals of Surgical Treatment and Research.2024; 106(1): 19. CrossRef - Clinical impact of coexistent chronic lymphocytic thyroiditis on central lymph node metastasis in low- to intermediate-risk papillary thyroid carcinoma: The MASTER study
Da Beom Heo, Ho-Ryun Won, Kyung Tae, Yea Eun Kang, Eonju Jeon, Yong Bae Ji, Jae Won Chang, June Young Choi, Hyeong Won Yu, Eu Jeong Ku, Eun Kyung Lee, Mijin Kim, Jun-Ho Choe, Bon Seok Koo
Surgery.2024; 175(4): 1049. CrossRef - Dynamic Changes in Treatment Response af-ter 131I in Differentiated Thyroid Cancer and Their Relationship with Recurrence Risk Stratification and TNM Staging
璐 狄
Advances in Clinical Medicine.2024; 14(03): 1083. CrossRef - ASO Author Reflections: Active Surveillance may be Possible in Patients with T1b Papillary Thyroid Carcinoma Over 55 Years of Age Without High-Risk Features on Preoperative Examinations
Ho-Ryun Won, Eonju Jeon, Da Beom Heo, Jae Won Chang, Minho Shong, Je Ryong Kim, Hyemi Ko, Yea Eun Kang, Hyon-Seung Yi, Ju Hee Lee, Kyong Hye Joung, Ji Min Kim, Younju Lee, Sung-Woo Kim, Young Ju Jeong, Yong Bae Ji, Kyung Tae, Bon Seok Koo
Annals of Surgical Oncology.2023; 30(4): 2254. CrossRef - Outcomes and Trends of Treatments in High‐Risk Differentiated Thyroid Cancer
Arash Abiri, Khodayar Goshtasbi, Sina J. Torabi, Edward C. Kuan, William B. Armstrong, Tjoson Tjoa, Yarah M. Haidar
Otolaryngology–Head and Neck Surgery.2023; 168(4): 745. CrossRef - Current Controversies in Low-Risk Differentiated Thyroid Cancer: Reducing Overtreatment in an Era of Overdiagnosis
Timothy M Ullmann, Maria Papaleontiou, Julie Ann Sosa
The Journal of Clinical Endocrinology & Metabolism.2023; 108(2): 271. CrossRef - Age-Dependent Clinicopathological Characteristics of Patients with T1b Papillary Thyroid Carcinoma: Implications for the Possibility of Active Surveillance
Ho-Ryun Won, Eonju Jeon, Da Beom Heo, Jae Won Chang, Minho Shong, Je Ryong Kim, Hyemi Ko, Yea Eun Kang, Hyon-Seung Yi, Ju Hee Lee, Kyong Hye Joung, Ji Min Kim, Younju Lee, Sung-Woo Kim, Young Ju Jeong, Yong Bae Ji, Kyung Tae, Bon Seok Koo
Annals of Surgical Oncology.2023; 30(4): 2246. CrossRef - Potential impact of obesity on the aggressiveness of low- to intermediate-risk papillary thyroid carcinoma: results from a MASTER cohort study
Mijin Kim, Yae Eun Kang, Young Joo Park, Bon Seok Koo, Eu Jeong Ku, June Young Choi, Eun Kyung Lee, Bo Hyun Kim
Endocrine.2023; 82(1): 134. CrossRef - Differentiated thyroid cancer: a focus on post-operative thyroid hormone replacement and thyrotropin suppression therapy
Benjamin J. Gigliotti, Sina Jasim
Endocrine.2023; 83(2): 251. CrossRef - Thyroid stimulating hormone suppression and recurrence after thyroid lobectomy for papillary thyroid carcinoma
Mi Rye Bae, Sung Hoon Nam, Jong-Lyel Roh, Seung-Ho Choi, Soon Yuhl Nam, Sang Yoon Kim
Endocrine.2022; 75(2): 487. CrossRef - The Concept of Economic Evaluation and Its Application in Thyroid Cancer Research
Kyungsik Kim, Mijin Kim, Woojin Lim, Bo Hyun Kim, Sue K. Park
Endocrinology and Metabolism.2021; 36(4): 725. CrossRef
- Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study)

- Clinical Study
- A Phase II Multi-Center, Non-Randomized, Parallel Group, Non-Inferiority Study to Compare the Efficacy of No Radioactive Iodine Remnant Ablation to Remnant Ablation Treatment in Low- to Intermediate-Risk of Papillary Thyroid Cancer: The MOREthyroid Trial Protocol
- Eun Kyung Lee, You Jin Lee, Young Joo Park, Jae Hoon Moon, Ka Hee Yi, Koon Soon Kim, Joo Hee Lee, Sun Wook Cho, Jungnam Joo, Yul Hwangbo, Sujeong Go, Do Joon Park
- Endocrinol Metab. 2020;35(3):571-577. Published online September 22, 2020
- DOI: https://doi.org/10.3803/EnM.2020.681
- 4,636 View
- 119 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
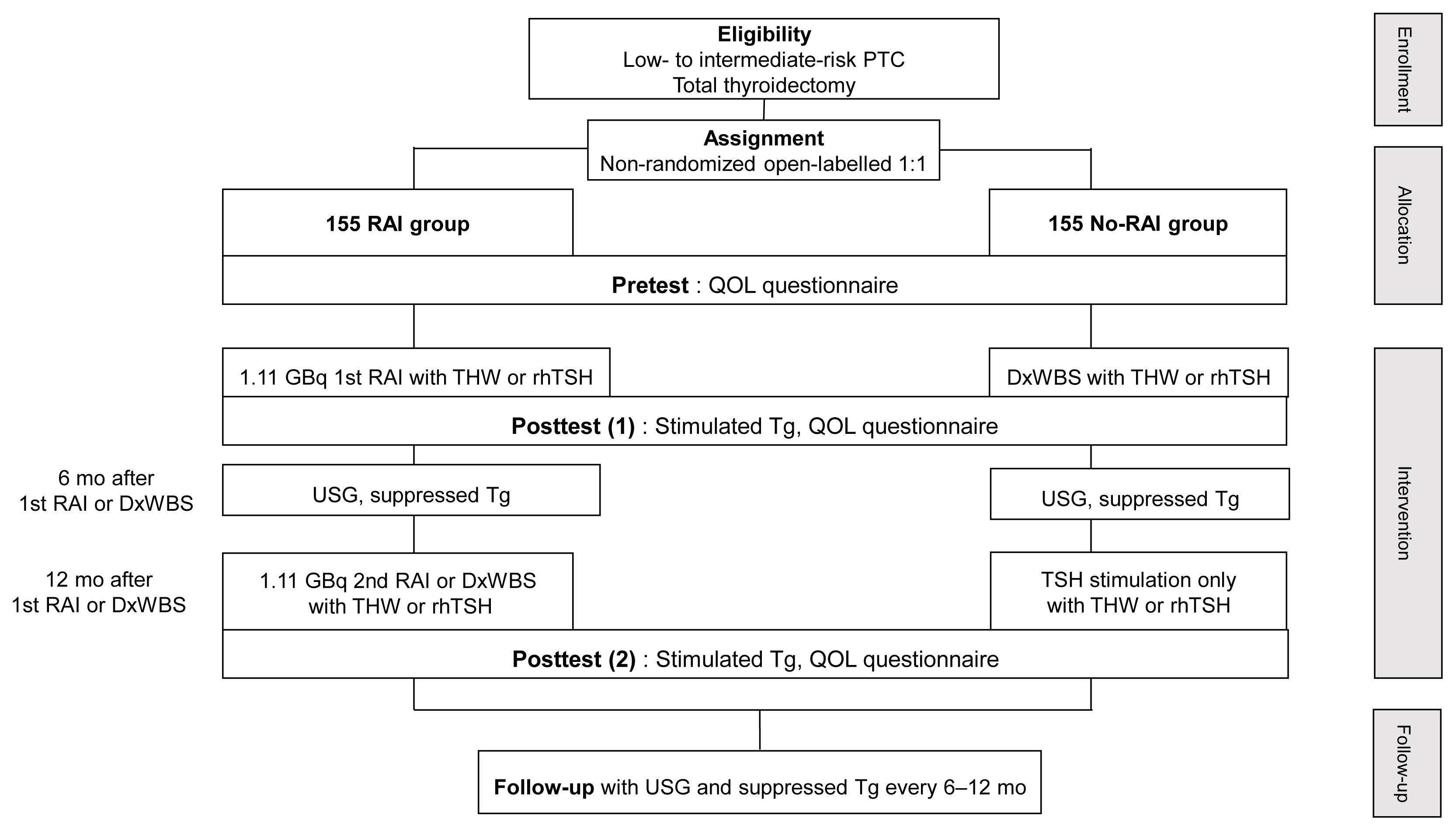
Radioactive iodine (RAI) remnant ablation is recommended in patients with papillary thyroid cancer (PTC) and extrathyroidal extension or central lymph node metastasis. However, there exists little evidence about the necessity of remnant ablation in PTC patients with low- to intermediate-risk, those have been increasing in recent decades.
Methods
This multicenter, prospective, non-randomized, parallel group clinical trial will enroll 310 eligible patients with low- to intermediate-risk of thyroid cancer. Inclusion criteria are patients who recently underwent total thyroidectomy for PTC with 3 or less tumors of size 1≤ to ≤2 cm with no microscopic extension and N0/x, or size ≤2 cm with microscopic extension and/or N1a (number of lymph node ≤3, size of tumor foci ≤0.2 cm, and lymph node ratio <0.4). Patients choose to undergo RAI ablation (131I, dose 1.1 GBq) or diagnostic whole-body scan (DxWBS) (131I or 123I, dose 0.074 to 0.222 GBq), followed by subsequent measurement of stimulated thyroglobulin (sTg) within 1 year. Survey for quality of life (QOL) will be performed at baseline and at 1 year after follow-up. The total enrollment period is 5 years, and patients will be followed up for 1 year. The primary endpoint is the non-inferiority of surgery alone to surgery with ablation in terms of biochemical remission (BCR) rate (sTg ≤2 ng/mL) without evidence of structural recurrence. The secondary endpoint was the difference of QOL.
Conclusion
This study will evaluate whether surgery alone achieves similar BCR and improved QOL compared to RAI ablation in patients with low- to intermediate-risk PTC within 1 year.

- Assay of Thyrotropin Receptor Antibodies with Recombinant Human Thyrotropin Receptor Expressed on Chinese Hamster Ovary Cells.
- Bo Youn Cho, Hong Kyu Lee, Chang Soon Koh, Jae Hoon Chung, Ka Hee Yi, Kyung Soo Ko, Won Bae Kim
- J Korean Endocr Soc. 1995;10(4):347-361. Published online November 7, 2019
- 1,166 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - Thyroid stimulating antibody which results in the development of hyperthyroidism and goiter in Graves' patients used to be measured by using rat thyroid cells, FRTL-5. However, this assay has disadvantages: decreased sensitivity due to differences in species, and fastidious culture conditions for FRTL-5 cells. Thus, we recently created stably transfected Chinese hamster ovary(CHO) cells containing the human TSH receptor(hTSHR-CHO) and developed optimal conditions for the measurement of thyroid stimulating antibody using hTSHR-CHO cells. In this study, to evaluate the clinical relevance of thyroid stimulating antibody measurement using hTSHR-CHO cells, we measured thyroid stimulating antibody activities of IgGs from Graves' disease and other thyroid disease using hTSHR-CHO cells, and compared to those of thyroid stimulating antibody assays using FRTL-5 cells. 1) The cut off value of positive thyroid stimulating antibody activity measured in hTSHR-CHO cells was 145%(above the mean +2SD) which was lower than 165% in FRTL-5 cells. The intra-assay and inter-assay variances were 3.9% to 9.0% and 12.7% to 1.6%, respectively. 2) Thyroid stimulating antibody activity was detected in 90% of patients with untreated Graves' disease when patients initially presented. Further, in patients seen initially but already under therapy, 75% had positive values if they were hyperthyroid but only 43% had IgGs with activity if they were euthyroid. Patients in clinical remission after therapy showed positive values in 23% of cases. Only 2 of 25 patients with Hashimoto's thyroiditis showed weak thyroid stimulating antibody activity, none of 18 patients with nodular nontoxie goiter, 1 of 15 patients with primary myxedema, and 2 of 33 control patients with no thyroid disease. Thus, the detection frequency and specificity of the assay with hTSHR-CHO cells was excellent for this type bioassay.3) The detection frequency of thyroid stimulating antibody activity by hTSHR-CHO cells assay system(90%) was higher than that by FRTL-5 cells assay system(66%) in untreated Graves' patients. Those two activities were positively correlated with each other(r=0.52, p<0.001). However, some IgGs showed discrepancy of the thyroid stimulating antibody activity measured in hTSHR-CHO cells and in FRTL-5 cells; 56 of 87 patients were positive in both cells system, 8 of 87 were negative in both cells system, 1 of 87 was only positive in FRTL-5 cells and 22 of 87 were only positive in hTSHR-CHO cell system. Thus, 73%(22/30) of IgGs showing negative values of thyroid stimulating antibody activities in FRTL-5 cells were detected its activities in hTSHR-CHO cells system.In summary, thyroid stimulating antibody assay with hTSHR-CHO cells exhibited so excellent sensitivity and specificity that this technique should be used for clinical practice as well as basic research.

- Thyroid Stimulating Antibody Assay with Chinese Hamster Ovary Cells Expressing Human Thyroid Stimulating Hormone (TSH) Receptor; Optimization of Assay Condition.
- Bo Youn Cho, Hong Kyu Lee, Young Kee Shong, Chang Soon Koh, Ka Hee Yi, Yeon Sahng Oh, Won Bae Kim
- J Korean Endocr Soc. 1995;10(4):333-346. Published online November 7, 2019
- 1,064 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - We investigated the optimal condition of thyroid stimulating antibody(TSAb) assay using Chinese hamster ovary cells transfected with cDNA of human TSH receptor(TSHr-CHO) stably expressing functional TSH receptors. The extracellular cAMP responses of TSHr-CHO cells to the stimulation of bTSH or Graves' IgG were observed in three different incubation media. Stimulation indices of extracellular cAMP were higher when sucrose containing NaCl-free isotonic Hank's balanced salt solution(HBSS)(media A)was used as incubation media than those of NaCl-free hypotonic HBSS(media B) or those of NaCl containing isotonic HBSS(media C). The incubation of TSHr-CHO cells in media B caused marked increase in the basal cAMP level without concomittant fold-increase in the stimulated cAMP level at various doses of bTSH and Graves' IgG. Decreasing the stimulation indices of extracellular cAMP, use of media B failed to detect TSAb activities in two TSAb-positive Graves' IgG tested. In case of media C, extracellular cAMP responses are poor at 0.001 and 0.1U/L of bTSH and at all doses of Graves' IgG tested(0.5, 1, 5g/L). The incubation of TSHr-CHO cells in media B caused significant increase in the number of trypan blue-stained, nonviable cells(5.7+-1.5, 7.6+-1.9 and 8.5+-1.6% at 1, 2 and 3h of incubation, respectively; p<0.01) comparing to those incubated in media A or media C(about 2-3% in both media). Those decrease in the viability of TSHr-CHO cells when incubated in hypotonic incubation media may explain the decrease in the stimulation index of extracellular cAMP with the use of media B in contrast to the case of FRTL-5 cells. TSAb assay of 87 consecutive fresh Graves' patients with TSHr-CHO cells using media A detected TSAb activities in 90%(78 patients) of them, and moreover TSAb activities showed significant positive correlation with the pre-treatment serum T_3 and free T_4 levels of those patients. We conclude that TSAb assay with TSHr-CHO cells is a sensitive and physiologically relevant assay system to measure TSAb activities merely through measurements of extracellular cAMP provided that the cells are incubated in NaCl-free isotonic incubation media.

- A Case of Addison's Disease due to Tuberculosis.
- Ji Young Kim, Ho Choon Jeon, Kyeong Young Kim, Sung Eun Cha, Hyung Seok Choi, In Sohn, Ka Hee Yi
- J Korean Endocr Soc. 1994;10(3):306-310. Published online November 6, 2019
- 1,077 View
- 36 Download
-
 Abstract
Abstract
 PDF
PDF - We reported a case of Addison's disease due to tuberculosis, which was pathologically confirmed by fine-needle aspiration biopsy. In a 39-year-old man with fatigue, weakness, and generalized cutaneous pigmentation, the diagnosis of Addison's disease was made by the finding of elevated plasma ACTH level and subnormal response to rapid ACTH test. Computed tomographic scan revealed bilateral adrenal mass with heterogenous uptake and peripheral rim enhancement, and calcification. Ultrasoundguided fine-deedle aspiration biopsy of the left adrenal mass disclosed granulomatous inflammation with caseation necrosis. The patient also had active tuberculosis in the right inguinal lymph node.

- Miscellaneous
- Corrigendum: Author's Name Correction. Study Protocol of Multicenter Prospective Cohort Study of Active Surveillance on Papillary Thyroid Microcarcinoma (MAeSTro)
- Jae Hoon Moon, Ji-hoon Kim, Eun Kyung Lee, Kyu Eun Lee, Sung Hye Kong, Yeo Koon Kim, Woo-Jin Jeong, Chang Yoon Lee, Roh-Eul Yoo, Yul Hwangbo, Young Shin Song, Min Joo Kim, Sun Wook Cho, Su-jin Kim, Eun-Jae Chung, June Young Choi, Chang Hwan Ryu, You Jin Lee, Jeong Hun Hah, Yuh-Seog Jung, Junsun Ryu, Yunji Hwang, Sue K. Park, Ho Kyung Sung, Ka Hee Yi, Do Joon Park, Young Joo Park
- Endocrinol Metab. 2018;33(3):427. Published online August 14, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.3.427
- 3,505 View
- 48 Download
- 2 Web of Science
- 2 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- Invasiveness and Metastatic Aggressiveness in Small Differentiated Thyroid Cancers: Demography of Small Papillary Thyroid Carcinomas in the Swedish Population
Haytham Bayadsi, Martin Bergman, Malin Sund, Joakim Hennings
World Journal of Surgery.2020; 44(2): 461. CrossRef - Clinical and pathologic predictors of lymph node metastasis in papillary thyroid microcarcinomas
Ling Zhao, Xiaoya Sun, Yukun Luo, Fulin Wang, Zhaohui Lyu
Annals of Diagnostic Pathology.2020; 49: 151647. CrossRef
- Invasiveness and Metastatic Aggressiveness in Small Differentiated Thyroid Cancers: Demography of Small Papillary Thyroid Carcinomas in the Swedish Population

- Thyroid
- Study Protocol of Multicenter Prospective Cohort Study of Active Surveillance on Papillary Thyroid Microcarcinoma (MAeSTro)
- Jae Hoon Moon, Ji-hoon Kim, Eun Kyung Lee, Kyu Eun Lee, Sung Hye Kong, Yeo Koon Kim, Woo-jin Jung, Chang Yoon Lee, Roh-Eul Yoo, Yul Hwangbo, Young Shin Song, Min Joo Kim, Sun Wook Cho, Su-jin Kim, Eun Jae Jung, June Young Choi, Chang Hwan Ryu, You Jin Lee, Jeong Hun Hah, Yuh-Seog Jung, Junsun Ryu, Yunji Hwang, Sue K. Park, Ho Kyung Sung, Ka Hee Yi, Do Joon Park, Young Joo Park
- Endocrinol Metab. 2018;33(2):278-286. Published online June 21, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.2.278
- 5,438 View
- 88 Download
- 34 Web of Science
- 31 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background The ongoing Multicenter Prospective Cohort Study of Active Surveillance on Papillary Thyroid Microcarcinoma (MAeSTro) aims to observe the natural course of papillary thyroid microcarcinoma (PTMC), develop a protocol for active surveillance (AS), and compare the long-term prognosis, quality of life, and medical costs between the AS and immediate surgery groups.
Methods This multicenter prospective cohort study of PTMC started in June 2016. The inclusion criteria were suspicious of malignancy or malignancy based on fine needle aspiration or core needle biopsy, age of ≥18 years, and a maximum diameter of ≤1 cm. If there was no major organ involvement, no lymph node/distant metastasis, and no variants with poor prognosis, the patients were explained of the pros and cons of immediate surgery and AS before selecting AS or immediate surgery. Follow-up visits (physical examination, ultrasonography, thyroid function, and questionnaires) are scheduled every 6 months during the first 2 years, and then every 1 year thereafter. Progression was defined as a maximum diameter increase of ≥3, ≥2 mm in two dimensions, suspected organ involvement, or lymph node/distant metastasis.
Results Among 439 enrolled patients, 290 patients (66.1%) chose AS and 149 patients (33.9%) chose immediate surgery. The median follow-up was 6.7 months (range, 0.2 to 11.9). The immediate surgery group had a larger maximum tumor diameter, compared to the AS group (7.1±1.9 mm vs. 6.6±2.0 mm, respectively;
P =0.014).Conclusion The results will be useful for developing an appropriate PTMC treatment policy based on its natural course and risk factors for progression.
-
Citations
Citations to this article as recorded by- Psychological adjustment to initial treatment for low‐risk thyroid cancer: Preliminary study
Gabriella T. Seo, Mark L. Urken, Lauren E. Wein, Michael P. Saturno, Danielle Kapustin, Monica H. Xing, Lauren E. Yue, Eric M. Dowling, Tracey A. Revenson, Katherine J. Roberts, Robert Michael Tuttle
Head & Neck.2023; 45(2): 439. CrossRef - Response to Letter to the Editor on Surgical Outcomes in Patients With Low-Risk Papillary Thyroid Microcarcinoma From MAeSTro Study: Immediate Operation Versus Delayed Operation Following Active Surveillance: A Multicenter Prospective Cohort Study
Hyeonuk Hwang, June Young Choi, Jae Hoon Moon, Eun Kyung Lee, Young Joo Park, Su-jin Kim, Yuh-Seog Jung
Annals of Surgery Open.2023; 4(3): e311. CrossRef - Lower Thyroid Cancer Mortality in Patients Detected by Screening: A Meta-Analysis
Shinje Moon, Young Shin Song, Kyong Yeun Jung, Eun Kyung Lee, Young Joo Park
Endocrinology and Metabolism.2023; 38(1): 93. CrossRef - To Screen or Not to Screen?
Do Joon Park
Endocrinology and Metabolism.2023; 38(1): 69. CrossRef - Surgical Outcomes in Patients With Low-risk Papillary Thyroid Microcarcinoma From MAeSTro Study
Hyeonuk Hwang, June Young Choi, Hyeong Won Yu, Jae Hoon Moon, Ji-hoon Kim, Eun Kyung Lee, Yeo Koon Kim, Chang Yoon Lee, Sun Wook Cho, Eun-Jae Chung, Chang Hwan Ryu, Junsun Ryu, Ka Hee Yi, Do Joon Park, Kyu Eun Lee, Young Joo Park, Su-jin Kim, Yuh-Seog Jun
Annals of Surgery.2023; 278(5): e1087. CrossRef - US Predictors of Papillary Thyroid Microcarcinoma Progression at Active Surveillance
Ji Ye Lee, Ji-hoon Kim, Yeo Koon Kim, Chang Yoon Lee, Eun Kyung Lee, Jae Hoon Moon, Hoon Sung Choi, Hwangbo Yul, Sun Wook Cho, Su-jin Kim, Kyu Eun Lee, Do Joon Park, Young Joo Park
Radiology.2023;[Epub] CrossRef - MET-receptor targeted fluorescent imaging and spectroscopy to detect multifocal papillary thyroid cancer
Madelon J. H. Metman, Pascal K. C. Jonker, Luc H. J. Sondorp, Bettien M. van Hemel, Mark S. Sywak, Anthony J. Gill, Liesbeth Jansen, Paul J. van Diest, Tessa M. van Ginhoven, Clemens W. G. M. Löwik, Anh H. Nguyen, Dominic J. Robinson, Gooitzen M. van Dam,
European Journal of Nuclear Medicine and Molecular Imaging.2023;[Epub] CrossRef - Active Surveillance of Thyroid Microcarcinomas: a Critical View
Claudio R. Cernea, Leandro Luongo Matos, Cecília Eugênio, Giovanna Mattos Ferreira, Yasmin Sa Cerqueira, Ana Kober N. Leite, Felipe A. B. Vanderlei, Dorival de Carlucci, Renato N. Gotoda, Flávio C. Hojaij, Vergilius J. F. Araújo-Filho
Current Oncology Reports.2022; 24(1): 69. CrossRef - Active Surveillance Versus Thyroid Surgery for Differentiated Thyroid Cancer: A Systematic Review
Roger Chou, Tracy Dana, Megan Haymart, Angela M. Leung, Ralph P. Tufano, Julie Ann Sosa, Matthew D. Ringel
Thyroid.2022; 32(4): 351. CrossRef - A Review of Active Surveillance of Papillary Thyroid Microcarcinoma
Cho Rok Lee
Journal of Endocrine Surgery.2022; 22(1): 1. CrossRef - Active Surveillance Versus Immediate Surgery for Low-Risk Papillary Thyroid Microcarcinoma Patients in South Korea: A Cost-Minimization Analysis from the MAeSTro Study
Kyungsik Kim, June Young Choi, Su-jin Kim, Eun Kyung Lee, Young Ki Lee, Jun Sun Ryu, Kyu Eun Lee, Jae Hoon Moon, Young Joo Park, Sun Wook Cho, Sue K. Park
Thyroid.2022; 32(6): 648. CrossRef - A cross-sectional survey of patient treatment choice in a multicenter prospective cohort study on active surveillance of papillary thyroid microcarcinoma (MAeSTro)
Yul Hwangbo, June Young Choi, Eun Kyung Lee, Chang Hwan Ryu, Sun Wook Cho, Eun Jae Chung, Jeong Hun Hah, Woo-Jin Jeong, Sue K. Park, Yuh-Seog Jung, Ji-hoon Kim, Min Joo Kim, Su-jin Kim, Yeo Koon Kim, Chang Yoon Lee, Ji Ye Lee, You Jin Lee, Hyeong Won Yu,
Thyroid.2022;[Epub] CrossRef - Progression of Low-Risk Papillary Thyroid Microcarcinoma During Active Surveillance: Interim Analysis of a Multicenter Prospective Cohort Study of Active Surveillance on Papillary Thyroid Microcarcinoma in Korea
Eun Kyung Lee, Jae Hoon Moon, Yul Hwangbo, Chang Hwan Ryu, Sun Wook Cho, June Young Choi, Eun-Jae Chung, Woo-Jin Jeong, Yuh-Seog Jung, Junsun Ryu, Su-jin Kim, Min Joo Kim, Yeo Koon Kim, Chang Yoon Lee, Ji Ye Lee, Hyeong Won Yu, Jeong Hun Hah, Kyu Eun Lee,
Thyroid.2022; 32(11): 1328. CrossRef - Indications and Strategy for Active Surveillance of Adult Low-Risk Papillary Thyroid Microcarcinoma: Consensus Statements from the Japan Association of Endocrine Surgery Task Force on Management for Papillary Thyroid Microcarcinoma
Iwao Sugitani, Yasuhiro Ito, Dai Takeuchi, Hirotaka Nakayama, Chie Masaki, Hisakazu Shindo, Masanori Teshima, Kazuhiko Horiguchi, Yusaku Yoshida, Toshiharu Kanai, Mitsuyoshi Hirokawa, Kiyomi Y. Hames, Isao Tabei, Akira Miyauchi
Thyroid.2021; 31(2): 183. CrossRef - Effect of Initial Treatment Choice on 2-year Quality of Life in Patients with Low-risk Papillary Thyroid Microcarcinoma
Jae Hoon Moon, Chang Hwan Ryu, Sun Wook Cho, June Young Choi, Eun-Jae Chung, Jeong Hun Hah, Yul Hwangbo, Woo-Jin Jeong, Yuh-Seog Jung, Ji-hoon Kim, Min Joo Kim, Su-jin Kim, Yeo Koon Kim, Chang Yoon Lee, Eun Kyung Lee, Ji Ye Lee, Kyu Eun Lee, You Jin Lee,
The Journal of Clinical Endocrinology & Metabolism.2021; 106(3): 724. CrossRef - Adoption of Active Surveillance for Very Low-Risk Differentiated Thyroid Cancer in the United States: A National Survey
Susan C Pitt, Nan Yang, Megan C Saucke, Nicholas Marka, Bret Hanlon, Kristin L Long, Alexandria D McDow, J P Brito, Benjamin R Roman
The Journal of Clinical Endocrinology & Metabolism.2021; 106(4): 1728. CrossRef - Protocol for a Korean Multicenter Prospective Cohort Study of Active Surveillance or Surgery (KoMPASS) in Papillary Thyroid Microcarcinoma
Min Ji Jeon, Yea Eun Kang, Jae Hoon Moon, Dong Jun Lim, Chang Yoon Lee, Yong Sang Lee, Sun Wook Kim, Min-Hee Kim, Bo Hyun Kim, Ho-Cheol Kang, Minho Shong, Sun Wook Cho, Won Bae Kim
Endocrinology and Metabolism.2021; 36(2): 359. CrossRef - Multifocality and Progression of Papillary Thyroid Microcarcinoma During Active Surveillance
Ryuta Nagaoka, Aya Ebina, Kazuhisa Toda, Tomoo Jikuzono, Marie Saitou, Masaomi Sen, Hiroko Kazusaka, Mami Matsui, Keiko Yamada, Hiroki Mitani, Iwao Sugitani
World Journal of Surgery.2021; 45(9): 2769. CrossRef - Active Surveillance as an Effective Management Option for Low-Risk Papillary Thyroid Microcarcinoma
Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Endocrinology and Metabolism.2021; 36(4): 717. CrossRef - The Concept of Economic Evaluation and Its Application in Thyroid Cancer Research
Kyungsik Kim, Mijin Kim, Woojin Lim, Bo Hyun Kim, Sue K. Park
Endocrinology and Metabolism.2021; 36(4): 725. CrossRef - Genomic and Transcriptomic Characteristics According to Size of Papillary Thyroid Microcarcinoma
Young Shin Song, Byung-Hee Kang, Seungbok Lee, Seong-Keun Yoo, Young Sik Choi, Jungsun Park, Dong Yoon Park, Kyu Eun Lee, Jeong-Sun Seo, Young Joo Park
Cancers.2020; 12(5): 1345. CrossRef - Experience with Active Surveillance of Thyroid Low-Risk Carcinoma in a Developing Country
Alvaro Sanabria
Thyroid.2020; 30(7): 985. CrossRef - Association of Patient Age With Progression of Low-risk Papillary Thyroid Carcinoma Under Active Surveillance
Alexandra Koshkina, Rouhi Fazelzad, Iwao Sugitani, Akira Miyauchi, Lehana Thabane, David P. Goldstein, Sangeet Ghai, Anna M. Sawka
JAMA Otolaryngology–Head & Neck Surgery.2020; 146(6): 552. CrossRef - Active surveillance in low risk papillary thyroid carcinoma
Fabian Pitoia, Anabella Smulever
World Journal of Clinical Oncology.2020; 11(6): 320. CrossRef - Early Diagnosis of Low-Risk Papillary Thyroid Cancer Results Rather in Overtreatment Than a Better Survival
Jolanta Krajewska, Aleksandra Kukulska, Malgorzata Oczko-Wojciechowska, Agnieszka Kotecka-Blicharz, Katarzyna Drosik-Rutowicz, Malgorzata Haras-Gil, Barbara Jarzab, Daria Handkiewicz-Junak
Frontiers in Endocrinology.2020;[Epub] CrossRef - The dilemma of papillary thyroid microcarcinoma management. To operate or not to operate, that is the question
Juan C Galofré
Endocrinología, Diabetes y Nutrición.2019; 66(8): 469. CrossRef - Computed Tomography for Detecting Cervical Lymph Node Metastasis in Patients Who Have Papillary Thyroid Microcarcinoma with Tumor Characteristics Appropriate for Active Surveillance
Dong-Hwa Lee, Yeo Koon Kim, Hyeong Won Yu, June Young Choi, So Yeon Park, Jae Hoon Moon
Thyroid.2019; 29(11): 1653. CrossRef - The dilemma of papillary thyroid microcarcinoma management. To operate or not to operate, that is the question
Juan C Galofré
Endocrinología, Diabetes y Nutrición (English ed.).2019; 66(8): 469. CrossRef - Longitudinal Assessment of Quality of Life According to Treatment Options in Low-Risk Papillary Thyroid Microcarcinoma Patients: Active Surveillance or Immediate Surgery (Interim Analysis of MAeSTro)
Sung Hye Kong, Junsun Ryu, Min Joo Kim, Sun Wook Cho, Young Shin Song, Ka Hee Yi, Do Joon Park, Yul Hwangbo, You Jin Lee, Kyu Eun Lee, Su-jin Kim, Woo-Jin Jeong, Eun-Jae Chung, Jeong Hun Hah, June Young Choi, Chang Hwan Ryu, Yuh-Seog Jung, Jae Hoon Moon,
Thyroid.2019; 29(8): 1089. CrossRef - Ultrasound-guided percutaneous laser ablation for papillary thyroid microcarcinoma: a retrospective analysis of 37 patients
Lili Ji, Qin Wu, Jun Gu, Xuedong Deng, Wei Zhou, Xing Fan, Feng Zhou
Cancer Imaging.2019;[Epub] CrossRef - Evolving management considerations in active surveillance for micropapillary thyroid carcinoma
Allen S. Ho, Irene Chen, Michelle Melany, Wendy L. Sacks
Current Opinion in Endocrinology, Diabetes & Obesity.2018; 25(5): 353. CrossRef
- Psychological adjustment to initial treatment for low‐risk thyroid cancer: Preliminary study

- Thyroid
- Star-Shaped Intense Uptake of 131I on Whole Body Scans Can Reflect Good Therapeutic Effects of Low-Dose Radioactive Iodine Treatment of 1.1 GBq
- Sung Hye Kong, Jung Ah Lim, Young Shin Song, Shinje Moon, Ye An Kim, Min Joo Kim, Sun Wook Cho, Jae Hoon Moon, Ka Hee Yi, Do Joon Park, Bo Youn Cho, Young Joo Park
- Endocrinol Metab. 2018;33(2):228-235. Published online May 4, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.2.228
- 5,300 View
- 50 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background After initial radioactive iodine (RAI) treatment in differentiated thyroid cancer patients, we sometimes observe a star-shaped region of intense uptake of 131I on whole body scans (WBSs), called a ‘star artifact.’ We evaluated the clinical implications of star artifacts on the success rate of remnant ablation and long-term prognosis.
Methods Total 636 patients who received 131I dose of 1.1 GBq for the initial RAI therapy and who did not show distant metastasis at the time of diagnosis were retrospectively evaluated. A negative second WBS was used for evaluating the ablation efficacy of the RAI therapy. Among them, 235 patients (36.9%) showed a star artifact on their first WBS.
Results In patients with first stimulated thyroglobulin (sTg) levels ≤2 ng/mL, patients with star artifacts had a higher rate of negative second WBS compared with those without star artifacts (77.8% vs. 63.9%,
P =0.044), and showed significantly higher recurrence-free survival (P =0.043) during the median 8.0 years (range, 1.0 to 10.0) of follow-up. The 5- and 10-year recurrence rates (5YRR, 10YRR) were also significantly lower in patients with star artifacts compared with those without (0% vs. 4.9%, respectively,P =0.006 for 5YRR; 0% vs. 6.4%, respectively,P =0.005 for 10YRR). However, ablation success rate or recurrence-free survival was not different among patients whose first sTg levels >2 ng/mL regardless of star artifacts.Conclusion Therefore, star artifacts at initial RAI therapy imply a good ablation efficacy or a favorable long-term prognosis in patients with sTg levels ≤2 ng/mL.
-
Citations
Citations to this article as recorded by- Prognostic value of star-shaped intense uptake of 131I in thyroid cancer patients
Liu Xiao, Wen Jie Zhang, Yue Qi Wang, Lin Li
Revista Española de Medicina Nuclear e Imagen Molecular (English Edition).2021; 40(1): 30. CrossRef - Valores pronósticos de la captación en estrella de 131I en pacientes con cáncer diferenciado de tiroides
L. Xiao, W.J. Zhang, Y.Q. Wang, L. Li
Revista Española de Medicina Nuclear e Imagen Molecular.2021; 40(1): 30. CrossRef - Comparison between planar and single-photon computed tomography images for radiation intensity quantification in iodine-131 scintigraphy
Yusuke Iizuka, Tomohiro Katagiri, Minoru Inoue, Kiyonao Nakamura, Takashi Mizowaki
Scientific Reports.2021;[Epub] CrossRef
- Prognostic value of star-shaped intense uptake of 131I in thyroid cancer patients

- Thyroid
- The Revised 2016 Korean Thyroid Association Guidelines for Thyroid Nodules and Cancers: Differences from the 2015 American Thyroid Association Guidelines
- Ka Hee Yi
- Endocrinol Metab. 2016;31(3):373-378. Published online September 26, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.3.373
- 7,351 View
- 177 Download
- 90 Web of Science
- 85 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Increased detection of thyroid nodules using high-resolution ultrasonography has resulted in a world-wide increase in the incidence of differentiated thyroid cancer (DTC). Despite the steep increase in its incidence, the age-standardized mortality rate of thyroid cancer has remained stable, which leads toward a trend of more conservative treatment. The latest American Thyroid Association (ATA) guidelines for thyroid nodules and thyroid cancer revised in 2015 suggested that fine needle aspiration biopsy should be performed for thyroid nodules larger than 1 cm and lobectomy might be sufficient for 1 to 4 cm intrathyroidal DTC. In addition, active surveillance instead of immediate surgical treatment was also recommended as a treatment option for papillary thyroid microcarcinoma based on the results of a few observational studies from Japan. The Korean Thyroid Association (KTA) has organized a task force team to develop revised guidelines for thyroid nodules and DTC after an extensive review of articles and intense discussion on whether we should accept the changes in the 2015 ATA guidelines. This paper introduces and discusses the updated major issues and differences in the ATA and the KTA guidelines.
-
Citations
Citations to this article as recorded by- Intraoperative pathologic evaluation of central compartment lymph nodes in patients undergoing lobectomy for unilateral papillary thyroid carcinoma
Hye Lim Bae, Jong-hyuk Ahn, JungHak Kwak, Hyun Soo Kim, Sang Gab Yoon, Jin Wook Yi, Su-jin Kim, Kyu Eun Lee
Asian Journal of Surgery.2024; 47(1): 360. CrossRef - Global scientific trends on thyroid disease in early 21st century: a bibliometric and visualized analysis
Mingyuan Song, Wei Sun, Qi Liu, Zhongqing Wang, Hao Zhang
Frontiers in Endocrinology.2024;[Epub] CrossRef - A Narrative Review of the 2023 Korean Thyroid Association Management Guideline for Patients with Thyroid Nodules
Eun Kyung Lee, Young Joo Park, Chan Kwon Jung, Dong Gyu Na
Endocrinology and Metabolism.2024; 39(1): 61. CrossRef - Lowering Barriers to Health Risk Assessments in Promoting Personalized Health Management
Hayoung Park, Se Young Jung, Min Kyu Han, Yeonhoon Jang, Yeo Rae Moon, Taewook Kim, Soo-Yong Shin, Hee Hwang
Journal of Personalized Medicine.2024; 14(3): 316. CrossRef - Clinicopathological Features and Molecular Signatures of Lateral Neck Lymph Node Metastasis in Papillary Thyroid Microcarcinoma
Jinsun Lim, Han Sai Lee, Jin-Hyung Heo, Young Shin Song
Endocrinology and Metabolism.2024; 39(2): 324. CrossRef - Prognostic Utility of Tumor Stage versus American Thyroid Association Risk Class in Thyroid Cancer
Arash Abiri, Jonathan Pang, Karthik R. Prasad, Khodayar Goshtasbi, Edward C. Kuan, William B. Armstrong, Yarah M. Haidar, Tjoson Tjoa
The Laryngoscope.2023; 133(1): 205. CrossRef - Active surveillance for PTMC warranted for the UK population?
Pavithran Maniam, Noah Harding, Lucy Li, Richard Adamson, Ashley Hay, Ian Nixon
Clinical Otolaryngology.2023; 48(1): 88. CrossRef - Cost-effectiveness of active surveillance versus early surgery for thyroid micropapillary carcinoma based on diagnostic and treatment norms in China
Min Lai, Miao Miao Zhang, Qing Qing Qin, Yu An, Yan Ting Li, Wen Zhen Yuan
Frontiers in Endocrinology.2023;[Epub] CrossRef - Biopsy strategies for intermediate and high suspicion thyroid nodules with macrocalcifications
Sungmok Kim, Jae Ho Shin, Yon Kwon Ihn
Current Medical Research and Opinion.2023; 39(2): 179. CrossRef - Active surveillance versus immediate surgery: A comparison of clinical and quality of life outcomes among patients with highly suspicious thyroid nodules 1 cm or smaller in China
Chunhao Liu, Hao Zhao, Yu Xia, Yue Cao, Liyang Zhang, Ya Zhao, Luying Gao, Ruifeng Liu, Yuewu Liu, Hongfeng Liu, Zhilan Meng, Shuzhou Liu, Ying Lu, Xiaoyi Li
European Journal of Surgical Oncology.2023; 49(9): 106917. CrossRef - SThy-Net: a feature fusion-enhanced dense-branched modules network for small thyroid nodule classification from ultrasound images
Abdulrhman H. Al-Jebrni, Saba Ghazanfar Ali, Huating Li, Xiao Lin, Ping Li, Younhyun Jung, Jinman Kim, David Dagan Feng, Bin Sheng, Lixin Jiang, Jing Du
The Visual Computer.2023; 39(8): 3675. CrossRef - Response to Letter to the Editor on Surgical Outcomes in Patients With Low-Risk Papillary Thyroid Microcarcinoma From MAeSTro Study: Immediate Operation Versus Delayed Operation Following Active Surveillance: A Multicenter Prospective Cohort Study
Hyeonuk Hwang, June Young Choi, Jae Hoon Moon, Eun Kyung Lee, Young Joo Park, Su-jin Kim, Yuh-Seog Jung
Annals of Surgery Open.2023; 4(3): e311. CrossRef - The Association of Pregnancy with Disease Progression in Patients Previously Treated for Differentiated Thyroid Cancer: A Propensity Score-Matched Retrospective Cohort Study
Xin Li, Wu-Cai Xiao, Fang Mei, Rui Shan, Shi-Bing Song, Bang-Kai Sun, He-Ling Bao, Jing Chen, Chun-Hui Yuan, Zheng Liu
Journal of Women's Health.2023; 32(11): 1174. CrossRef - Mortality rate and causes of death in papillary thyroid microcarcinoma
Jung Heo, Hyun Jin Ryu, Hyunju Park, Tae Hyuk Kim, Sun Wook Kim, Young Lyun Oh, Jae Hoon Chung
Endocrine.2023; 83(3): 671. CrossRef - Surgical Outcomes in Patients With Low-risk Papillary Thyroid Microcarcinoma From MAeSTro Study
Hyeonuk Hwang, June Young Choi, Hyeong Won Yu, Jae Hoon Moon, Ji-hoon Kim, Eun Kyung Lee, Yeo Koon Kim, Chang Yoon Lee, Sun Wook Cho, Eun-Jae Chung, Chang Hwan Ryu, Junsun Ryu, Ka Hee Yi, Do Joon Park, Kyu Eun Lee, Young Joo Park, Su-jin Kim, Yuh-Seog Jun
Annals of Surgery.2023; 278(5): e1087. CrossRef - US Predictors of Papillary Thyroid Microcarcinoma Progression at Active Surveillance
Ji Ye Lee, Ji-hoon Kim, Yeo Koon Kim, Chang Yoon Lee, Eun Kyung Lee, Jae Hoon Moon, Hoon Sung Choi, Hwangbo Yul, Sun Wook Cho, Su-jin Kim, Kyu Eun Lee, Do Joon Park, Young Joo Park
Radiology.2023;[Epub] CrossRef - Bilaterality as a Risk Factor for Recurrence in Papillary Thyroid Carcinoma
Hyeji Kim, Hyungju Kwon
Cancers.2023; 15(22): 5414. CrossRef - Clinical and molecular genetic analysis of cytologically uncertain thyroid nodules in patients with thyroid disease
Jindrich Lukas, Barbora Hintnausova, Vlasta Sykorova, Martin Syrucek, Marek Maly, David Lukas, Jaroslava Duskova
Biomedical Papers.2023;[Epub] CrossRef - Thyroid Papillary Microcarcinoma - Carcinoma with Clinically Benign Behaviour
Hitesh R Singhavi, Manish Mair, Burhanuddin Qayyumi, Arjun Singh, Pankaj Chaturvedi
Journal of Head & Neck Physicians and Surgeons.2023; 11(2): 95. CrossRef - Trends in Diagnosis of Noninvasive Follicular Thyroid Neoplasm With Papillarylike Nuclear Features and Total Thyroidectomies for Patients With Papillary Thyroid Neoplasms
Lisa Caulley, Antoine Eskander, Weining Yang, Edel Auh, Lydia Cairncross, Nancy L. Cho, Bahar Golbon, Subramania Iyer, Jeffrey C. Liu, Paul J. Lee, Brenessa Lindeman, Charles Meltzer, Nicole Molin, Alessandra Moore, Julia Noel, Halie Nozolino, Jesse Paste
JAMA Otolaryngology–Head & Neck Surgery.2022; 148(2): 99. CrossRef - What's in a Name? A Cost-Effectiveness Analysis of the Noninvasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features' Nomenclature Revision
Vikas Mehta, Ankita Naraparaju, David Liao, Louise Davies, Bryan R. Haugen, Peter A. Kopp, Susan J. Mandel, Yuri E. Nikiforov, Douglas S. Ross, Jennifer J. Shin, R. Michael Tuttle, Gregory W. Randolph
Thyroid.2022; 32(4): 421. CrossRef - Clinical management of low-risk papillary thyroid microcarcinoma
Chie MASAKI, Kiminori SUGINO, Koichi ITO
Minerva Endocrinology.2022;[Epub] CrossRef - Can Active Surveillance Management be Developed for Patients With Low-Risk Papillary Thyroid Microcarcinoma? A Preliminary Investigation in a Chinese Population
Wen Liu, Weihan Cao, Zhizhong Dong, Ruochuan Cheng
Endocrine Practice.2022; 28(4): 391. CrossRef - Assessment of Radiofrequency Ablation for Papillary Microcarcinoma of the Thyroid
Sam P. J. van Dijk, Hannelore I. Coerts, Sabrina T. G. Gunput, Evert F. S. van Velsen, Marco Medici, Adriaan Moelker, Robin P. Peeters, Cornelis Verhoef, Tessa M. van Ginhoven
JAMA Otolaryngology–Head & Neck Surgery.2022; 148(4): 317. CrossRef - The Future of Thyroid Nodule Risk Stratification
Nydia Burgos, Naykky Singh Ospina, Jennifer A. Sipos
Endocrinology and Metabolism Clinics of North America.2022; 51(2): 305. CrossRef - Complication Rates of Total Thyroidectomy vs Hemithyroidectomy for Treatment of Papillary Thyroid Microcarcinoma
Vivian Hsiao, Tyler J. Light, Abdullah A. Adil, Michael Tao, Alexander S. Chiu, Mary Hitchcock, Natalia Arroyo, Sara Fernandes-Taylor, David O. Francis
JAMA Otolaryngology–Head & Neck Surgery.2022; 148(6): 531. CrossRef - Malignancy risk stratification of thyroid nodules smaller than 10 mm with ACR-TIRADS, K-TIRADS, and ATA-2015 guidelines: a prospective study
Mehrdad Nabahati, Zoleika Moazezi
Egyptian Journal of Radiology and Nuclear Medicine.2022;[Epub] CrossRef - Thyroglobulin-Based Risk Factor Repositioning for Determining Radioactive Iodine Activity in Patients with Papillary Thyroid Carcinoma: a Multicenter Retrospective Cohort Study
Subin Jeon, Seong Young Kwon, Sang-Woo Lee, Sang Kyun Bae
Nuclear Medicine and Molecular Imaging.2022; 56(4): 173. CrossRef - Quality of Life of Survivors of Thyroid Cancer Is Not Inferior to That in Subjects without Cancer: Long-Term after Over 5 Years
Jeongmin Lee, Youn-Ju Lee, Dong-Jun Lim, Jung-Min Lee, Sang-Ah Chang, Min-Hee Kim
Endocrinology and Metabolism.2022; 37(4): 664. CrossRef - Residual, regrowth, and new growth of radiofrequency ablation for benign thyroid nodules of different volumes: two-year follow-up results
Meng-Hsiang Chen, Wei-Che Lin, Sheng-Dean Luo, Pi-Ling Chiang, Yueh-Sheng Chen, Wei-Chih Chen, An-Ni Lin, Cheng-Kang Wang, Jung-Hwan Baek, Hsiu-Ling Chen
International Journal of Hyperthermia.2022; 39(1): 1172. CrossRef - Progression of Low-Risk Papillary Thyroid Microcarcinoma During Active Surveillance: Interim Analysis of a Multicenter Prospective Cohort Study of Active Surveillance on Papillary Thyroid Microcarcinoma in Korea
Eun Kyung Lee, Jae Hoon Moon, Yul Hwangbo, Chang Hwan Ryu, Sun Wook Cho, June Young Choi, Eun-Jae Chung, Woo-Jin Jeong, Yuh-Seog Jung, Junsun Ryu, Su-jin Kim, Min Joo Kim, Yeo Koon Kim, Chang Yoon Lee, Ji Ye Lee, Hyeong Won Yu, Jeong Hun Hah, Kyu Eun Lee,
Thyroid.2022; 32(11): 1328. CrossRef - Recent Changes in the Incidence of Thyroid Cancer in Korea between 2005 and 2018: Analysis of Korean National Data
Yun Mi Choi, Jiwoo Lee, Mi Kyung Kwak, Min Ji Jeon, Tae Yong Kim, Eun-Gyoung Hong, Won Bae Kim, Won Gu Kim
Endocrinology and Metabolism.2022; 37(5): 791. CrossRef - Strain Versus 2D Shear-Wave Elastography Parameters—Which Score Better in Predicting Thyroid Cancer?
Andreea Borlea, Ioan Sporea, Alexandru Popa, Mihnea Derban, Laura Taban, Dana Stoian
Applied Sciences.2022; 12(21): 11147. CrossRef - Estimating the risk of completion total thyroidectomy using real-world data to guide initial surgical decision-making for patients with clinical low-risk papillary thyroid carcinoma
Wen Liu, Xiangxiang Zhan, Zhizhong Dong, Yanjun Su, Jianming Zhang, Jun Qian, Yunhai Ma, Chang Diao, Ruochuan Cheng
Holistic Integrative Oncology.2022;[Epub] CrossRef - Rigorous radiofrequency ablation can completely treat low-risk small papillary thyroid carcinoma without affecting subsequent surgical management
Xinyang Li, Jie Li, Zhi Qiao, Lin Yan, Jing Xiao, Yingying Li, Mingbo Zhang, Yukun Luo
European Radiology.2022; 33(6): 4189. CrossRef - Whirling technique for thyroid fine needle aspiration biopsy: a preliminary study of effectiveness and safety
Jae Ho Shin, Seung Wan Han, Hyang Lim Lee, Yon Kwon Ihn
Ultrasonography.2021; 40(1): 147. CrossRef - Value of dual-phase, contrast-enhanced CT combined with ultrasound for the diagnosis of metastasis to central lymph nodes in patients with papillary thyroid cancer
Ying Liu, Sheng Li, Cuiju Yan, Caiyun He, Miao Yun, Min Liu, Jianhua Zhou, Longzhong Liu
Clinical Imaging.2021; 75: 5. CrossRef - Clinical outcomes of T4a papillary thyroid cancer with recurrent laryngeal nerve involvement: a retrospective analysis
Han-Seul Na, Hyun-Keun Kwon, Sung-Chan Shin, Yong-Il Cheon, Myeonggu Seo, Jin-Choon Lee, Eui-Suk Sung, Minhyung Lee, In-Joo Kim, Bo Hyun Kim, Byung-Joo Lee
Scientific Reports.2021;[Epub] CrossRef - Protocol for a Korean Multicenter Prospective Cohort Study of Active Surveillance or Surgery (KoMPASS) in Papillary Thyroid Microcarcinoma
Min Ji Jeon, Yea Eun Kang, Jae Hoon Moon, Dong Jun Lim, Chang Yoon Lee, Yong Sang Lee, Sun Wook Kim, Min-Hee Kim, Bo Hyun Kim, Ho-Cheol Kang, Minho Shong, Sun Wook Cho, Won Bae Kim
Endocrinology and Metabolism.2021; 36(2): 359. CrossRef - Thyroid nodules in childhood‐onset Hashimoto's thyroiditis: Frequency, risk factors, follow‐up course and genetic alterations of thyroid cancer
Yun Jeong Lee, Yeon Jin Cho, You Joung Heo, Eun‐Jae Chung, Young Hun Choi, Jong‐Il Kim, Young Joo Park, Choong Ho Shin, Young Ah Lee
Clinical Endocrinology.2021; 95(4): 638. CrossRef - Clinical implications of age and excellent response to therapy in patients with high‐risk differentiated thyroid carcinoma
Meihua Jin, Jonghwa Ahn, Yu‐Mi Lee, Tae‐Yon Sung, Dong Eun Song, Tae Yong Kim, Ki‐Wook Chung, Jin‐Sook Ryu, Won Bae Kim, Young Kee Shong, Min Ji Jeon, Won Gu Kim
Clinical Endocrinology.2021; 95(6): 882. CrossRef - Ecografía clínica de la glándula tiroides y del cuello
Pepa Bertrán Culla, David Teixidó Gimeno, Pere Guirado Vila
FMC - Formación Médica Continuada en Atención Primaria.2021; 28(7): 390. CrossRef - Active Surveillance as an Effective Management Option for Low-Risk Papillary Thyroid Microcarcinoma
Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Endocrinology and Metabolism.2021; 36(4): 717. CrossRef - Clinical Effects of Microwave Ablation in the Treatment of Low-Risk Papillary Thyroid Microcarcinomas and Related Histopathological Changes
Chenya Lu, Xingjia Li, Xiaoqiu Chu, Ruiping Li, Jie Li, Jianhua Wang, Yalin Wang, Yang Xu, Guofang Chen, Shuhang Xu, Chao Liu
Frontiers in Endocrinology.2021;[Epub] CrossRef - Optimization of follow-up in patients with papillary thyroid cancer who show no evidence of disease 9–12 months after treatment
Fabian Nordell, Ghadir Hallal, Pernilla Asp, Martin Almquist
BJS Open.2021;[Epub] CrossRef - The most reliable time point for intact parathyroid hormone measurement to predict hypoparathyroidism after total thyroidectomy with central neck dissection to treat papillary thyroid carcinoma: a prospective cohort study
Jae Won Chang, Ki Wan Park, Seung-Nam Jung, Lihua Liu, Sung Min Kim, Bon Seok Koo
European Archives of Oto-Rhino-Laryngology.2020; 277(2): 549. CrossRef - Time Trends for Prostate Cancer Incidence from 2003 to 2013 in South Korea: An Age-Period-Cohort Analysis
Hyun Young Lee, Do Kyoung Kim, Seung Whan Doo, Won Jae Yang, Yun Seob Song, Bora Lee, Jae Heon Kim
Cancer Research and Treatment.2020; 52(1): 301. CrossRef - Clinical behavior and outcome of papillary T1 thyroid cancers: South Korea vs. Turkey vs. Colombia in a cohort study analyzing oncological outcomes
Murat Ozdemir, Yong-Sang Lee, Ozer Makay, Juan Pablo Dueñas, Bulent Yazici, Aysegul Akgun, Gokhan Icoz, Mahir Akyildiz, Soo Young Kim, Seok-Mo Kim, Hojin Chang, Hang-Seok Chang, Cheong Soo Park
Asian Journal of Surgery.2020; 43(8): 795. CrossRef - Radioiodine ablation in thyroid cancer patients: renal function and external radiation dose rate at discharge according to patient preparation
Yeon-Hee Han, Hwan-Jeong Jeong, Myung-Hee Sohn, Sun Y. Lee, Seok T. Lim
The Quarterly Journal of Nuclear Medicine and Molecular Imaging.2020;[Epub] CrossRef - Effect of the location and size of thyroid nodules on the diagnostic performance of ultrasound elastography: A retrospective analysis
Xinxin Xie, Yongqiang Yu
Clinics.2020; 75: e1720. CrossRef Fine-Needle Aspiration of Subcentimeter Thyroid Nodules in the Real-World Management
Chaiho Jeong, Hyunsam Kim, Jeongmin Lee, Jeonghoon Ha, Min-Hee Kim, Moo Il Kang, Dong-Jun Lim
Cancer Management and Research.2020; Volume 12: 7611. CrossRef- Continuing controversy regarding individualized surgical decision-making for patients with 1–4 cm low-risk differentiated thyroid carcinoma: A systematic review
Wen Liu, Xuejing Yan, Ruochuan Cheng
European Journal of Surgical Oncology.2020; 46(12): 2174. CrossRef - Clinical Implication of World Health Organization Classification in Patients with Follicular Thyroid Carcinoma in South Korea: A Multicenter Cohort Study
Meihua Jin, Eun Sook Kim, Bo Hyun Kim, Hee Kyung Kim, Hyon-Seung Yi, Min Ji Jeon, Tae Yong Kim, Ho-Cheol Kang, Won Bae Kim, Young Kee Shong, Mijin Kim, Won Gu Kim
Endocrinology and Metabolism.2020; 35(3): 618. CrossRef - Clinical Outcomes of N1b Papillary Thyroid Cancer Patients Treated with Two Different Doses of Radioiodine Ablation Therapy
Meihua Jin, Jonghwa Ahn, Yu-Mi Lee, Tae-Yon Sung, Won Gu Kim, Tae Yong Kim, Jin-Sook Ryu, Won Bae Kim, Young Kee Shong, Min Ji Jeon
Endocrinology and Metabolism.2020; 35(3): 602. CrossRef - A Propensity Score‐matched Comparison Study of Surgical Outcomes in Patients with Differentiated Thyroid Cancer After Robotic Versus Open Total Thyroidectomy
Dong Sik Bae, Do Hoon Koo
World Journal of Surgery.2019; 43(2): 540. CrossRef - Diagnostic value of cytology, thyroglobulin, and combination of them in fine-needle aspiration of metastatic lymph nodes in patients with differentiated thyroid cancer
Yixin Xu, Dapeng Wu, Wenting Wu, Jian Jiang, Cheng Xi, Nianyuan Ye, Yibo Wang, Xuezhong Xu
Medicine.2019; 98(45): e17859. CrossRef - Investigation of blood groups in benign thyroid diseases in Turkey
Murat Dağdeviren, İhsan Ateş, Burak Furkan Demir, Emine Ergün, Canan Yıldız, Mustafa Altay
Endocrine Journal.2019; 66(11): 1001. CrossRef - Tumor Volume Doubling Time in Active Surveillance of Papillary Thyroid Carcinoma
Hye-Seon Oh, Hyemi Kwon, Eyun Song, Min Ji Jeon, Tae Yong Kim, Jeong Hyun Lee, Won Bae Kim, Young Kee Shong, Ki-Wook Chung, Jung Hwan Baek, Won Gu Kim
Thyroid.2019; 29(5): 642. CrossRef - Tumor doubling time predicts response to sorafenib in radioactive iodine-refractory differentiated thyroid cancer
Min Joo Kim, Seok-Mo Kim, Eun Kyung Lee, Yul Hwangbo, You Jin Lee, Sun Wook Cho, Do Joon Park, Yumi Lee, Young Joo Park
Endocrine Journal.2019; 66(7): 597. CrossRef - Total thyroidectomy's association with survival in papillary thyroid cancers and the high proportion of total thyroidectomy in low-risk patients: Analysis of Korean nationwide data
Hyun-Soo Zhang, Eun-Kyung Lee, Yuh-Seog Jung, Byung-Ho Nam, Kyu-Won Jung, Hyun-Joo Kong, Young-Joo Won, Boyoung Park
Surgery.2019; 165(3): 629. CrossRef - Individualized Follow-Up Strategy for Patients with an Indeterminate Response to Initial Therapy for Papillary Thyroid Carcinoma
Hye-Seon Oh, Jong Hwa Ahn, Eyun Song, Ji Min Han, Won Gu Kim, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Min Ji Jeon
Thyroid.2019; 29(2): 209. CrossRef - Differentiated Thyroid Cancer and Radioactive Iodine: Past, Present and Future
Jaetae Lee, Il Jo
International Journal of Thyroidology.2019; 12(2): 71. CrossRef - Diagnostic performance of HMGA2 gene expression for differentiation of malignant thyroid nodules: A systematic review and meta‐analysis
Bo Hyun Kim, Seong Jang Kim, Mijin Kim, Sang‐Woo Lee, Shin Young Jeong, Kyoungjune Pak, Keunyoung Kim, In Joo Kim
Clinical Endocrinology.2018; 89(6): 856. CrossRef - Ultrasound risk evaluation of thyroid nodules that are “unspecified” in the 2015 American Thyroid Association management guidelines
Luying Gao, Xuehua Xi, Juanjuan Wang, Xiao Yang, Ying Wang, Shenling Zhu, Xingjian Lai, Xiaoyan Zhang, Ruina Zhao, Bo Zhang
Medicine.2018; 97(52): e13914. CrossRef - Refining the eighth edition AJCC TNM classification and prognostic groups for papillary thyroid cancer with lateral nodal metastasis
Hye In Kim, Kyunga Kim, So Young Park, Jun-Ho Choe, Jung-Han Kim, Jee Soo Kim, Young Lyun Oh, Soo Yeon Hahn, Jung Hee Shin, Hyeon Seon Ahn, Sun Wook Kim, Tae Hyuk Kim, Jae Hoon Chung
Oral Oncology.2018; 78: 80. CrossRef - Thyroid cancer surgery guidelines in an era of de-escalation
K.J. Kovatch, C.W. Hoban, A.G. Shuman
European Journal of Surgical Oncology.2018; 44(3): 297. CrossRef - Changes in Serum Thyroglobulin Levels After Lobectomy in Patients with Low-Risk Papillary Thyroid Cancer
Suyeon Park, Min Ji Jeon, Hye-Seon Oh, Yu-Mi Lee, Tae-Yon Sung, Minkyu Han, Ji Min Han, Tae Yong Kim, Ki-Wook Chung, Won Bae Kim, Young Kee Shong, Won Gu Kim
Thyroid.2018; 28(8): 997. CrossRef - Study Protocol of Multicenter Prospective Cohort Study of Active Surveillance on Papillary Thyroid Microcarcinoma (MAeSTro)
Jae Hoon Moon, Ji-hoon Kim, Eun Kyung Lee, Kyu Eun Lee, Sung Hye Kong, Yeo Koon Kim, Woo-jin Jung, Chang Yoon Lee, Roh-Eul Yoo, Yul Hwangbo, Young Shin Song, Min Joo Kim, Sun Wook Cho, Su-jin Kim, Eun Jae Jung, June Young Choi, Chang Hwan Ryu, You Jin Lee
Endocrinology and Metabolism.2018; 33(2): 278. CrossRef - Low-Dose Radioactive Iodine Ablation Is Sufficient in Patients With Small Papillary Thyroid Cancer Having Minor Extrathyroidal Extension and Central Lymph Node Metastasis (T3 N1a): Reply
Minjung Seo, Yon Seon Kim, Jong Cheol Lee, Myung Woul Han, Eun Sook Kim, Kyung Bin Kim, Seol Hoon Park
Clinical Nuclear Medicine.2018; 43(8): 635. CrossRef - Diagnosis and treatment of low-risk papillary thyroid microcarcinoma
Jae Hoon Moon, Young Joo Park
Journal of the Korean Medical Association.2018; 61(4): 232. CrossRef - Efficacy of a Home-Based Exercise Program After Thyroidectomy for Thyroid Cancer Patients
Kyunghee Kim, Mee Ock Gu, Jung Hwa Jung, Jong Ryeal Hahm, Soo Kyoung Kim, Jin Hyun Kim, Seung Hoon Woo
Thyroid.2018; 28(2): 236. CrossRef - Genome-Wide Association Study Reveals Distinct Genetic Susceptibility of Thyroid Nodules From Thyroid Cancer
Yul Hwangbo, Eun Kyung Lee, Ho-Young Son, Sun-Wha Im, Soo-Jung Kwak, Ji Won Yoon, Min Joo Kim, Jeongseon Kim, Hoon Sung Choi, Chang Hwan Ryu, You Jin Lee, Jong-Il Kim, Nam H Cho, Young Joo Park
The Journal of Clinical Endocrinology & Metabolism.2018; 103(12): 4384. CrossRef - Active Surveillance of Low-Risk Papillary Thyroid Microcarcinoma: A Multi-Center Cohort Study in Korea
Hye-Seon Oh, Jeonghoon Ha, Hye In Kim, Tae Hyuk Kim, Won Gu Kim, Dong-Jun Lim, Tae Yong Kim, Sun Wook Kim, Won Bae Kim, Young Kee Shong, Jae Hoon Chung, Jung Hwan Baek
Thyroid.2018; 28(12): 1587. CrossRef - Ultrasound criteria for risk stratification of thyroid nodules in the previously iodine deficient area of Austria - a single centre, retrospective analysis
Christina Tugendsam, Veronika Petz, Wolfgang Buchinger, Brigitta Schmoll-Hauer, Iris Pia Schenk, Karin Rudolph, Michael Krebs, Georg Zettinig
Thyroid Research.2018;[Epub] CrossRef - Practical Initial Risk Stratification Based on Lymph Node Metastases in Pediatric and Adolescent Differentiated Thyroid Cancer
Min Ji Jeon, Young Nam Kim, Tae-Yong Sung, Suck Joon Hong, Yoon Young Cho, Tae Yong Kim, Young Kee Shong, Won Bae Kim, Sun Wook Kim, Jae Hoon Chung, Tae Hyuk Kim, Won Gu Kim
Thyroid.2018; 28(2): 193. CrossRef - Current Radiological Approach in Thyroid Nodules
Duzgun Yildirim, Deniz Alis, Sabri Sirolu, Cesur Samanci, Fethi Emre Ustabasioglu, Bulent Colakoglu
Journal of Cancer Therapy.2017; 08(05): 423. CrossRef - A new paradigm in low-risk papillary microcarcinoma: active surveillance
Alex González Bóssolo, Michelle Mangual Garcia, Paula Jeffs González, Miosotis Garcia, Guillermo Villarmarzo, Jose Hernán Martinez
Endocrinology, Diabetes & Metabolism Case Reports.2017;[Epub] CrossRef - Serial Neck Ultrasonographic Evaluation of Changes in Papillary Thyroid Carcinoma During Pregnancy
Hye-Seon Oh, Won Gu Kim, Suyeon Park, Mijin Kim, Hyemi Kwon, Min Ji Jeon, Jeong Hyun Lee, Jung Hwan Baek, Dong Eun Song, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Thyroid.2017; 27(6): 773. CrossRef - Restratification of survival prognosis of N1b papillary thyroid cancer by lateral lymph node ratio and largest lymph node size
Hye In Kim, Tae Hyuk Kim, Jun‐Ho Choe, Jung‐Han Kim, Jee Soo Kim, Young Lyun Oh, Soo Yeon Hahn, Jung Hee Shin, Hye Won Jang, Young Nam Kim, Hosu Kim, Hyeon Seon Ahn, Kyunga Kim, Sun Wook Kim, Jae Hoon Chung
Cancer Medicine.2017; 6(10): 2244. CrossRef - Comparison on Fine Needle Aspiration Cytology (FNAC) and Thyroid Ultrasonography in Management of Thyroid Nodules
Sandini A Gunaratne
International Clinical Pathology Journal.2017;[Epub] CrossRef - Current Practices of Thyroid Fine-Needle Aspiration in Asia: A Missing Voice
Andrey Bychkov, Kennichi Kakudo, SoonWon Hong
Journal of Pathology and Translational Medicine.2017; 51(6): 517. CrossRef - Clinical outcomes after delayed thyroid surgery in patients with papillary thyroid microcarcinoma
Min Ji Jeon, Won Gu Kim, Hyemi Kwon, Mijin Kim, Suyeon Park, Hye-Seon Oh, Minkyu Han, Tae-Yon Sung, Ki-Wook Chung, Suck Joon Hong, Tae Yong Kim, Young Kee Shong, Won Bae Kim
European Journal of Endocrinology.2017; 177(1): 25. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - The Impact of Thyroid Nodule Size and Fine-Needle Aspiration Biopsy Result on the Risk of Malignancy in the Patients Who Underwent Thyroidectomy
Hwibin Im, Yu-Young Park, Jae-Gu Cho, Seung-Kuk Baek, Soon-Young Kwon, Kwang-Yoon Jung, Jeong-Soo Woo
Korean Journal of Otorhinolaryngology-Head and Neck Surgery.2017; 60(6): 308. CrossRef - Active Surveillance of Papillary Thyroid Microcarcinoma: A Mini-Review from Korea
Tae Yong Kim, Young Kee Shong
Endocrinology and Metabolism.2017; 32(4): 399. CrossRef
- Intraoperative pathologic evaluation of central compartment lymph nodes in patients undergoing lobectomy for unilateral papillary thyroid carcinoma

- Thyroid
- The Diagnosis and Management of Hyperthyroidism in Korea: Consensus Report of the Korean Thyroid Association
- Jae Hoon Moon, Ka Hee Yi
- Endocrinol Metab. 2013;28(4):275-279. Published online December 12, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.4.275
- 5,343 View
- 70 Download
- 54 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Hyperthyroidism is one of the causes of thyrotoxicosis and the most common cause of hyperthyroidism in Korea is Graves disease. The diagnosis and treatment of Graves disease are different according to geographical area. Recently, the American Thyroid Association and the American Association of Clinical Endocrinologists suggested new management guidelines for hyperthyroidism. However, these guidelines are different from clinical practice in Korea and are difficult to apply. Therefore, the Korean Thyroid Association (KTA) conducted a survey of KTA members regarding the diagnosis and treatment of hyperthyroidism, and reported the consensus on the management of hyperthyroidism. In this review, we summarized the KTA report on the contemporary practice patterns in the diagnosis and management of hyperthyroidism, and compared this report with guidelines from other countries.
-
Citations
Citations to this article as recorded by- Effect of previous administration of potassium iodine and different durations of low iodine diets for radioiodine therapy on the treatment of Graves' disease in iodine-rich areas
Mika Tamura, Kunihiro Nakada, Haruna Iwanaga, Naotoshi Fujita, Katsuhiko Kato
European Journal of Nuclear Medicine and Molecular Imaging.2024; 51(4): 1060. CrossRef - Effects of altitude on thyroid disorders according to Chinese three-rung, ladder-like topography: national cross-sectional study
Boshen Gong, Youmin Wang, Jin-an Zhang, Qiao Zhang, Jiajun Zhao, Jiashu Li, Xichang Wang, Yutong Han, Ziwei Yu, Chenyu Zhang, Bingcong Peng, Yumin Xing, Qiuxian Li, Ping Wang, Yongze Li, Weiping Teng, Zhongyan Shan
BMC Public Health.2024;[Epub] CrossRef - MACE and Hyperthyroidism Treated With Medication, Radioactive Iodine, or Thyroidectomy
Carol Chiung-Hui Peng, Yu-Jie Lin, Sun Y. Lee, Shu-Man Lin, Cheng Han, Ching-Hui Loh, Huei-Kai Huang, Elizabeth N. Pearce
JAMA Network Open.2024; 7(3): e240904. CrossRef - Increased risk of incident gout in patients with hyperthyroidism: a nationwide retrospective cohort study
Ju-Yeun Lee, So-Yeon Park, Seo Young Sohn
Rheumatology International.2023; 44(3): 451. CrossRef - The Current Status of Hyperthyroidism in Korea
Hyemi Kwon
Endocrinology and Metabolism.2023; 38(4): 392. CrossRef - A machine learning-assisted system to predict thyrotoxicosis using patients’ heart rate monitoring data: a retrospective cohort study
Kyubo Shin, Jongchan Kim, Jaemin Park, Tae Jung Oh, Sung Hye Kong, Chang Ho Ahn, Joon Ho Moon, Min Joo Kim, Jae Hoon Moon
Scientific Reports.2023;[Epub] CrossRef - Immunometabolic signatures predict recovery from thyrotoxic myopathy in patients with Graves' disease
Daiki Setoyama, Ho Yeop Lee, Ji Sun Moon, Jingwen Tian, Yea Eun Kang, Ju Hee Lee, Minho Shong, Dongchon Kang, Hyon‐Seung Yi
Journal of Cachexia, Sarcopenia and Muscle.2022; 13(1): 355. CrossRef - Comparison of 99mTc Pertechnetate Thyroid Uptake Rates by Gamma Probe and Gamma Camera Methods for Differentiating Graves’ Disease and Thyroiditis
Meihua Jin, Jonghwa Ahn, Seong-gil Jo, Jangwon Park, Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Jin-Sook Ryu
Nuclear Medicine and Molecular Imaging.2022; 56(1): 42. CrossRef - KSNM60 in Nuclear Endocrinology: from the Beginning to the Future
Chae Moon Hong, Young Jin Jeong, Hae Won Kim, Byeong-Cheol Ahn
Nuclear Medicine and Molecular Imaging.2022; 56(1): 17. CrossRef - Graves’ disease and the risk of Parkinson’s disease: a Korean population-based study
Yoon Young Cho, Bongseong Kim, Dong Wook Shin, Jinyoung Youn, Ji Oh Mok, Chul-Hee Kim, Sun Wook Kim, Jae Hoon Chung, Kyungdo Han, Tae Hyuk Kim
Brain Communications.2022;[Epub] CrossRef - Graves’ Disease and the Risk of End-Stage Renal Disease: A Korean Population-Based Study
Yoon Young Cho, Bongseong Kim, Dong Wook Shin, Hye Ryoun Jang, Bo-Yeon Kim, Chan-Hee Jung, Jae Hyeon Kim, Sun Wook Kim, Jae Hoon Chung, Kyungdo Han, Tae Hyuk Kim
Endocrinology and Metabolism.2022; 37(2): 281. CrossRef - Evaluation and Management of Bone Health in Patients with Thyroid Diseases: a Position Statement from the Korean Thyroid Association
A Ram Hong, Hwa Young Ahn, Bu Kyung Kim, Seong Hee Ahn, So Young Park, Min-Hee Kim, Jeongmin Lee, Sun Wook Cho, Ho-Cheol Kang
International Journal of Thyroidology.2022; 15(1): 1. CrossRef - Patient Population and Test Utilization for Thyroid Function in Local Clinics and Hospitals in Korea
Rihwa Choi, Sang Gon Lee, Eun Hee Lee
Diagnostics.2022; 12(7): 1638. CrossRef - 2021 Asia-Pacific Graves’ Disease Consortium Survey of Clinical Practice Patterns in the Management of Graves’ Disease
Rajeev Parameswaran, Mechteld Christine de Jong, James Lee Wai Kit, Kathleen Sek, Tran Quang Nam, Tran Viet Thang, Nguyen Thy Khue, Than Than Aye, Phone Myint Tun, Timothy Cole, Julie A. Miller, Michael Villa, Benjapa Khiewvan, Sirinart Sirinvaravong, Yon
Endocrine.2022; 79(1): 135. CrossRef - Graves’ disease, its treatments, and the risk of atrial fibrillation: A Korean population-based study
Yoon Young Cho, Bongseong Kim, Dughyun Choi, Chul-Hee Kim, Dong Wook Shin, Jee Soo Kim, Seung-Jung Park, Sun Wook Kim, Jae Hoon Chung, Kyungdo Han, Tae Hyuk Kim
Frontiers in Endocrinology.2022;[Epub] CrossRef - Forty Years Together, New Leap Forward! The 40th Anniversary of the Korean Endocrine Society
Jong Chul Won, Ki-Hyun Baek
Endocrinology and Metabolism.2022; 37(6): 851. CrossRef - Evaluation of the role of thyroid scintigraphy in the differential diagnosis of thyrotoxicosis
Carolina M. Perdomo, Marta García‐Goñi, Lidia Sancho, José J. Paricio, María D. Lozano, Magdalena de la Higuera, María Currás, Javier Arbizu, Juan C. Galofré
Clinical Endocrinology.2021; 94(3): 466. CrossRef - Treatment of patients with Graves’ disease in Sweden compared to international surveys of an ‘index patient’
Gabriel Sjölin, Kristina Byström, Mats Holmberg, Ove Törring, Selwan Khamisi, Jan Calissendorff, Mikael Lantz, Bengt Hallengren, Helena Filipsson Nyström, Tereza Planck, Göran Wallin
Endocrinology, Diabetes & Metabolism.2021;[Epub] CrossRef - Secular Trends in Ablation Therapy for Graves’ Disease: An Analysis of a 15-Year Experience at a Tertiary Hospital in South Korea
Min Joo Kim, Ye An Kim, Sun Wook Cho, Su-jin Kim, Kyu Eun Lee, Young Joo Park, Do Joon Park, Bo Youn Cho
Journal of Clinical Medicine.2021; 10(8): 1629. CrossRef - Long-Term Antithyroid Drug Treatment of Graves’ Disease in Children and Adolescents: A 20-Year Single-Center Experience
Ari Song, Su Jin Kim, Min-Sun Kim, Jiyeon Kim, Insung Kim, Ga Young Bae, Eunseop Seo, Young Seok Cho, Joon Young Choi, Sung Yoon Cho, Dong-Kyu Jin
Frontiers in Endocrinology.2021;[Epub] CrossRef - Association of Polygenetic Risk Scores Related to Immunity and Inflammation with Hyperthyroidism Risk and Interactions between the Polygenetic Scores and Dietary Factors in a Large Cohort
Mi Young Song, Sunmin Park, Anjali Mishra
Journal of Thyroid Research.2021; 2021: 1. CrossRef - Treatment Modality and Risk of Heart Failure in Patients With Long-Standing Graves’ Disease: A Nationwide Population-Based Cohort Study
Eyun Song, Mina Kim, Sojeong Park, Min Jeong Park, Jung A. Kim, Eun Roh, Ji Hee Yu, Nam Hoon Kim, Ji A. Seo, Sin Gon Kim, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
Frontiers in Endocrinology.2021;[Epub] CrossRef - Risk of Diabetes in Patients with Long-Standing Graves’ Disease: A Longitudinal Study
Eyun Song, Min Ji Koo, Eunjin Noh, Soon Young Hwang, Min Jeong Park, Jung A Kim, Eun Roh, Kyung Mook Choi, Sei Hyun Baik, Geum Joon Cho, Hye Jin Yoo
Endocrinology and Metabolism.2021; 36(6): 1277. CrossRef - Diabetes and Hyperthyroidism: Is There a Causal Link?
Sang Yong Kim
Endocrinology and Metabolism.2021; 36(6): 1175. CrossRef - Incidence and Mortality of Myocardial Infarction and Stroke in Patients with Hyperthyroidism: A Nationwide Cohort Study in Korea
Hyun Jung Kim, Taeuk Kang, Min Ji Kang, Hyeong Sik Ahn, Seo Young Sohn
Thyroid.2020; 30(7): 955. CrossRef - Diagnosis and Management of Graves’ Disease in Thailand: A Survey of Current Practice
Chutintorn Sriphrapradang
Journal of Thyroid Research.2020; 2020: 1. CrossRef - The success rate of radioactive iodine therapy for Graves’ disease in iodine-replete area and affecting factors: a single-center study
Hyunju Park, Hye In Kim, Jun Park, So Young Park, Tae Hyuk Kim, Jae Hoon Chung, Joon Young Choi, Sun Wook Kim
Nuclear Medicine Communications.2020; 41(3): 212. CrossRef - Tirotoksikoz nedenli erektil disfonksiyon üzerine sildenafil etkisinin histopatolojik olarak değerlendirilmesi
Murat ÖZDEMİR, Canberk TOMRUK, Gürkan YİĞİTTÜRK, Varlık EROL, Emel Öykü ÇETİN, Ilgın YILDIRIM ŞİMŞİR, Çiğdem YENİSEY, Yiğit UYANIKGİL, Adnan ŞİMŞİR, Özer MAKAY
Ege Tıp Dergisi.2020; 59(3): 215. CrossRef - The Management of Thyroid Disease in COVID-19 Pandemic
Won Sang Yoo, Hyun-Kyung Chung
International Journal of Thyroidology.2020; 13(2): 65. CrossRef - Is Hyperthyroidism Diagnosed and Treated Appropriately in the United States?
Ammar Asban, Sophie Dream, Brenessa Lindeman
Advances in Surgery.2019; 53: 117. CrossRef - Long-term remission following antithyroid drug withdrawal in patients with Graves’ hyperthyroidism: parameters with prognostic value
Ricardo V. García-Mayor, Paula Álvarez-Vázquez, Enrique Fluiters, Diana Valverde, Amalia Andrade
Endocrine.2019; 63(2): 316. CrossRef - Safety of long-term antithyroid drug treatment? A systematic review
F. Azizi, R. Malboosbaf
Journal of Endocrinological Investigation.2019; 42(11): 1273. CrossRef - Changes in Thyroid Peroxidase and Thyroglobulin Antibodies Might Be Associated with Graves' Disease Relapse after Antithyroid Drug Therapy
Yun Mi Choi, Mi Kyung Kwak, Sang Mo Hong, Eun-Gyoung Hong
Endocrinology and Metabolism.2019; 34(3): 268. CrossRef - Prevalence and Annual Incidence of Thyroid Disease in Korea from 2006 to 2015: A Nationwide Population-Based Cohort Study
Hyemi Kwon, Jin-hyung Jung, Kyung-Do Han, Yong-Gyu Park, Jung-Hwan Cho, Da Young Lee, Ji Min Han, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
Endocrinology and Metabolism.2018; 33(2): 260. CrossRef - An update in the treatment preference for hyperthyroidism
Obin Kwon
Nature Reviews Endocrinology.2018; 14(7): 438. CrossRef - Clinical Feasibility of Monitoring Resting Heart Rate Using a Wearable Activity Tracker in Patients With Thyrotoxicosis: Prospective Longitudinal Observational Study
Jie-Eun Lee, Dong Hwa Lee, Tae Jung Oh, Kyoung Min Kim, Sung Hee Choi, Soo Lim, Young Joo Park, Do Joon Park, Hak Chul Jang, Jae Hoon Moon
JMIR mHealth and uHealth.2018; 6(7): e159. CrossRef - Graves' Disease Patients with Large Goiters Respond Best to Radioactive Iodine Doses of at Least 15 mCi: a Sonographic Volumetric Study
Yun Ah Jeong, Jee Hee Yoon, Hee Kyung Kim, Ho-Cheol Kang
International Journal of Thyroidology.2018; 11(2): 137. CrossRef - Chylothorax Associated with Substernal Goiter in Graves’ Disease Treated with Radioactive Iodine
Seo Young Oh, Bo Hyun Kim, Do Young Kim, Kyu Min Lee, Min Jin Lee, Sung Su Kim, Jong Ho Kim, Yun Kyung Jeon, Sang Soo Kim, Yong Ki Kim, In Joo Kim
International Journal of Endocrinology and Metabolism.2017;[Epub] CrossRef - Vitiligo and overt thyroid diseases: A nationwide population-based study in Korea
Jung Min Bae, June Hyunkyung Lee, Jae Seung Yun, Byeol Han, Tae Young Han
Journal of the American Academy of Dermatology.2017; 76(5): 871. CrossRef - Increased risk of thyroid diseases in patients with systemic lupus erythematosus: A nationwide population-based Study in Korea
Jae-Seung Yun, Jung Min Bae, Ki-Jo Kim, Yu Seok Jung, Gyong Moon Kim, Hyung-Rae Kim, Jun-Seok Lee, Seung-Hyun Ko, Seon-Ah Cha, Yu-Bae Ahn, Ludmila Prokunina-Olsson
PLOS ONE.2017; 12(6): e0179088. CrossRef - The Second Antithyroid Drug Treatment Is Effective in Relapsed Graves' Disease Patients: A Median 11-Year Follow-Up Study
Ye An Kim, Sun Wook Cho, Hoon Sung Choi, Shinje Moon, Jae Hoon Moon, Kyung Won Kim, Do Joon Park, Ka Hee Yi, Young Joo Park, Bo Youn Cho
Thyroid.2017; 27(4): 491. CrossRef - Free Thyroxine, Anti-Thyroid Stimulating Hormone Receptor Antibody Titers, and Absence of Goiter Were Associated with Responsiveness to Methimazole in Patients with New Onset Graves' Disease
Hoon Sung Choi, Won Sang Yoo
Endocrinology and Metabolism.2017; 32(2): 281. CrossRef - Long-Term Antithyroid Drug Treatment: A Systematic Review and Meta-Analysis
Fereidoun Azizi, Ramin Malboosbaf
Thyroid.2017; 27(10): 1223. CrossRef - The Recurrence Rate of Graves' Disease among Patients with Subclinical Thyrotoxicosis after Initial Remission with Antithyroid Agents
Myoung Sook Shim, Soo Min Nam, Jin Sae Yoo, Hae Kyung Kim, Sang Jun Lee, Mi Young Lee
International Journal of Thyroidology.2017; 10(2): 77. CrossRef - Serum 25-hydroxyvitamin D might be an independent prognostic factor for Graves disease recurrence
Hwa Young Ahn, Yun Jae Chung, Bo Youn Cho
Medicine.2017; 96(31): e7700. CrossRef - Recent Advances in Autoimmune Thyroid Diseases
Won Sang Yoo, Hyun Kyung Chung
Endocrinology and Metabolism.2016; 31(3): 379. CrossRef - Usefulness of Measuring Thyroid Stimulating Antibody at the Time of Antithyroid Drug Withdrawal for Predicting Relapse of Graves Disease
Hyemi Kwon, Won Gu Kim, Eun Kyung Jang, Mijin Kim, Suyeon Park, Min Ji Jeon, Tae Yong Kim, Jin-Sook Ryu, Young Kee Shong, Won Bae Kim
Endocrinology and Metabolism.2016; 31(2): 300. CrossRef - Hyperthyroidism
Simone De Leo, Sun Y Lee, Lewis E Braverman
The Lancet.2016; 388(10047): 906. CrossRef - Differentiating Graves' disease from subacute thyroiditis using ratio of serum free triiodothyronine to free thyroxine
Chutintorn Sriphrapradang, Adikan Bhasipol
Annals of Medicine and Surgery.2016; 10: 69. CrossRef - Management of hyperthyroid patients in dental emergencies: a case report
Kyung-Jin Lee, Wonse Park, Nan-Sim Pang, Jin-Hyung Cho, Kee-Deog Kim, Bock Young Jung, Eun-Jung Kwak
Journal of Dental Anesthesia and Pain Medicine.2016; 16(2): 147. CrossRef - The Presence of Thyroid-Stimulation Blocking Antibody Prevents High Bone Turnover in Untreated Premenopausal Patients with Graves’ Disease
Sun Wook Cho, Jae Hyun Bae, Gyeong Woon Noh, Ye An Kim, Min Kyong Moon, Kyoung Un Park, Junghan Song, Ka Hee Yi, Do Joon Park, June-Key Chung, Bo Youn Cho, Young Joo Park, Jung-Eun Kim
PLOS ONE.2015; 10(12): e0144599. CrossRef - Refractory Graves' Disease Successfully Cured by Adjunctive Cholestyramine and Subsequent Total Thyroidectomy
Yeoree Yang, Seawon Hwang, Minji Kim, Yejee Lim, Min-Hee Kim, Sohee Lee, Dong-Jun Lim, Moo-Il Kang, Bong-Yun Cha
Endocrinology and Metabolism.2015; 30(4): 620. CrossRef - Improved quality of life in hyperthyroidism patients after surgery
Branka Bukvic, Vladan Zivaljevic, Sandra Sipetic, Aleksandar Diklic, Katarina Tausanovic, Dragos Stojanovic, Dejan Stevanovic, Ivan Paunovic
Journal of Surgical Research.2015; 193(2): 724. CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef
- Effect of previous administration of potassium iodine and different durations of low iodine diets for radioiodine therapy on the treatment of Graves' disease in iodine-rich areas


 KES
KES

 First
First Prev
Prev



